TRILLIANT HEALTH RESEARCH
Research
Timely trend analysis. Free in your inbox.
Receive weekly studies from Trilliant Health.
Cancer Survival Up 140% Since the Mid-1970s, but Mortality Improvements Are Uneven Across Racial Groups
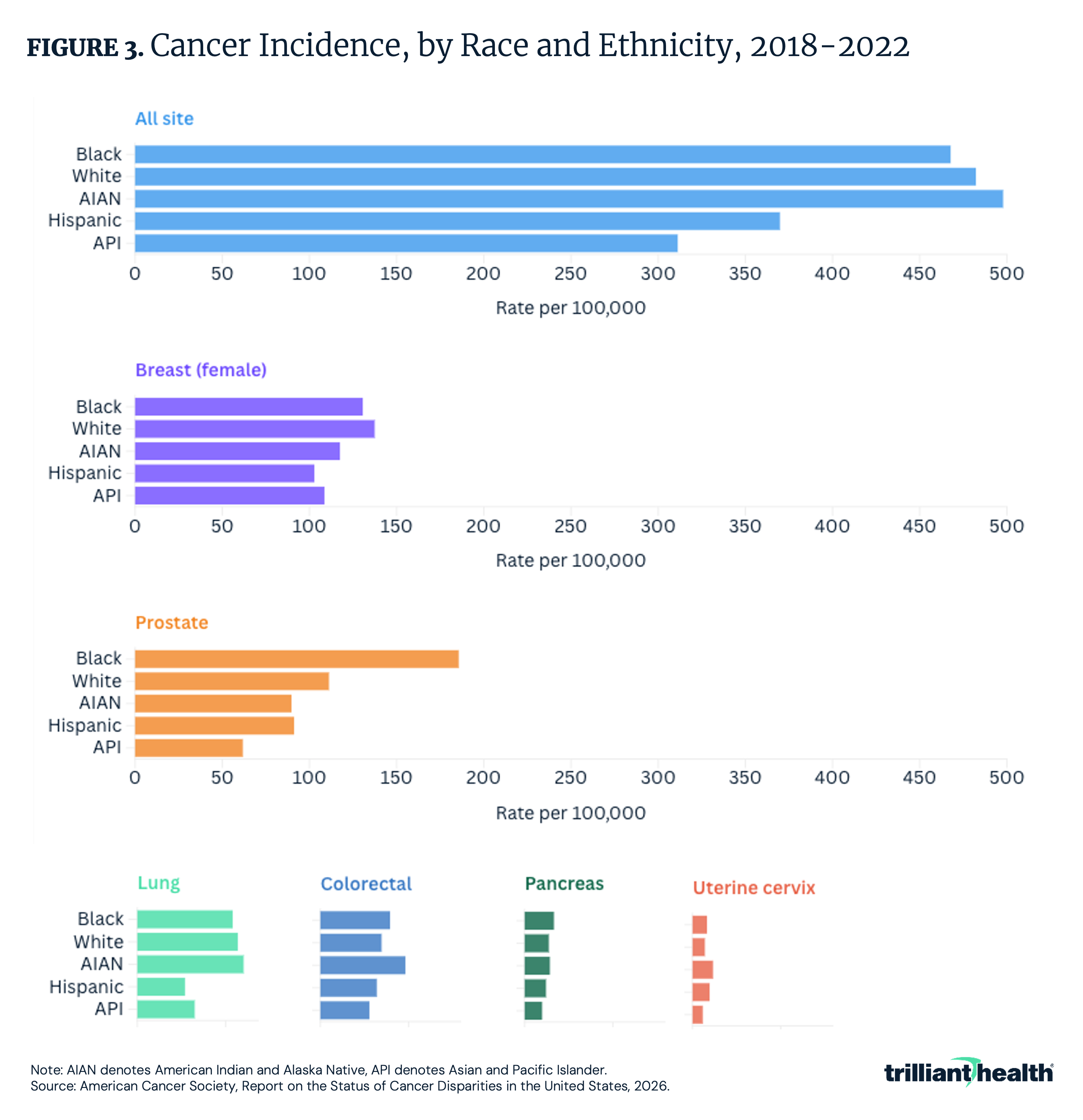
Five-year cancer survival has reached a milestone of 70% – up from 49% in the mid-1970s. But mortality improvements are uneven: Black and American Indian and Alaska Native individuals have disproportionately high mortality rates despite, in some cases, lower overall incidence.
February 26, 2026
Cancer Survival Up 140% Since the Mid-1970s, but Mortality Improvements Are Uneven Across Racial Groups
ACS projects 2.1M new cancer cases and 626,140 deaths in the U.S. for 2026. Five-year survival has reached 70%, but disparities persist by race, region and socioeconomic status.
Allison Oakes, Ph.D.
StudiesFebruary 19, 2026
Intra-Market Rate Variation Can Lead to Spending Differences that Exceed $102M for a Single Orthopedic Procedure in Dallas-Fort Worth
Health plan price transparency data reveals notable price variation for the same procedures, enabling employers to cut costs by steering employees to high-value providers and optimizing network choices.
Trilliant Health
StudiesFebruary 12, 2026
In the Same Market, Medicare Episodes of Care Can Range Up to 80x
Surgical volume for mandatory TEAM surgical procedures varies widely (one to 3,300 eligible Medicare procedures per hospital), while 30-day Medicare episode costs can differ up to 80x within the same market (e.g., $1,829 to $146,069 for a spinal fusion). These cost disparities exist despite minimal variation in quality. Even hospitals with strong occupancy and margins can exhibit inefficient downstream care. Consequently, TEAM reimbursement outcomes will be driven largely by cost management rather than quality differentiation.
Trilliant Health
StrategyFebruary 10, 2026
AI in Healthcare: Current Uses, Shared Challenges and Future Stakeholder Opportunities
As excitement around the healthcare applications of AI grows, understanding how health economy stakeholders are actually using AI, their challenges and future opportunities is crucial to navigate the rapidly shifting health economy.
Trilliant Health
StudiesFebruary 05, 2026
While Quality Is Relatively Comparable Across TEAM Hospitals, Financial Health Is Highly Variable
An analysis of 724 hospitals in CMS’s mandatory TEAM model, examining operating margins, readmissions, payer mix and more.
Trilliant Health
StudiesJanuary 29, 2026
More Americans Are Dying at Home but Hospital-Based Deaths Remain Most Common
Place of death in the U.S. is shifting: hospitals remain most common (34.6% in 2024), while deaths at home rose to 34.3% from 2018–2024.
Trilliant Health
FundamentalsJanuary 27, 2026
Middlemen in the U.S. Healthcare System: Shaping Costs and Complexity
Middlemen such PBMs, GPOs, TPAs and health insurance brokers play a central role in connecting stakeholders across healthcare, but their influence is increasingly under scrutiny for contributing to financial waste.
Trilliant Health
StudiesJanuary 22, 2026
Primary Care Panels Vary in Size Based on Demographic Factors and Employment Structure
Primary care patient panels vary widely across practice settings, with employment status emerging as a crucial indicator.
Trilliant Health
StudiesJanuary 15, 2026
Potential Revenue Impacts of Elimination of the Medicare Inpatient Only List
The average difference between IPPS and OPPS payment rates across all 285 procedures is -$16,334 per procedure.
Trilliant Health






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)
