Research
Despite Regulatory Scrutiny, Increases in Adult ADHD Diagnosis and Off-Label Stimulant Prescribing Continued Through 2023
July 14, 2025Study Takeaways
- While ADHD patient volume among children and adolescents (ages 0-17) declined relative to 2018, particularly among males, adult ADHD diagnoses (ages 18-49) increased, especially among females, up 61.7% in 2023.
- ADHD frequently co-occurs with a range of behavioral health conditions, most commonly anxiety and mood disorders.
- Since 2019, an increasing proportion of patients prescribed stimulants do not have a documented ADHD diagnosis. In 2018, 86.4% of stimulant recipients had an ADHD diagnosis in their medical claims, but by 2023, this percentage had dropped to 57.0%.
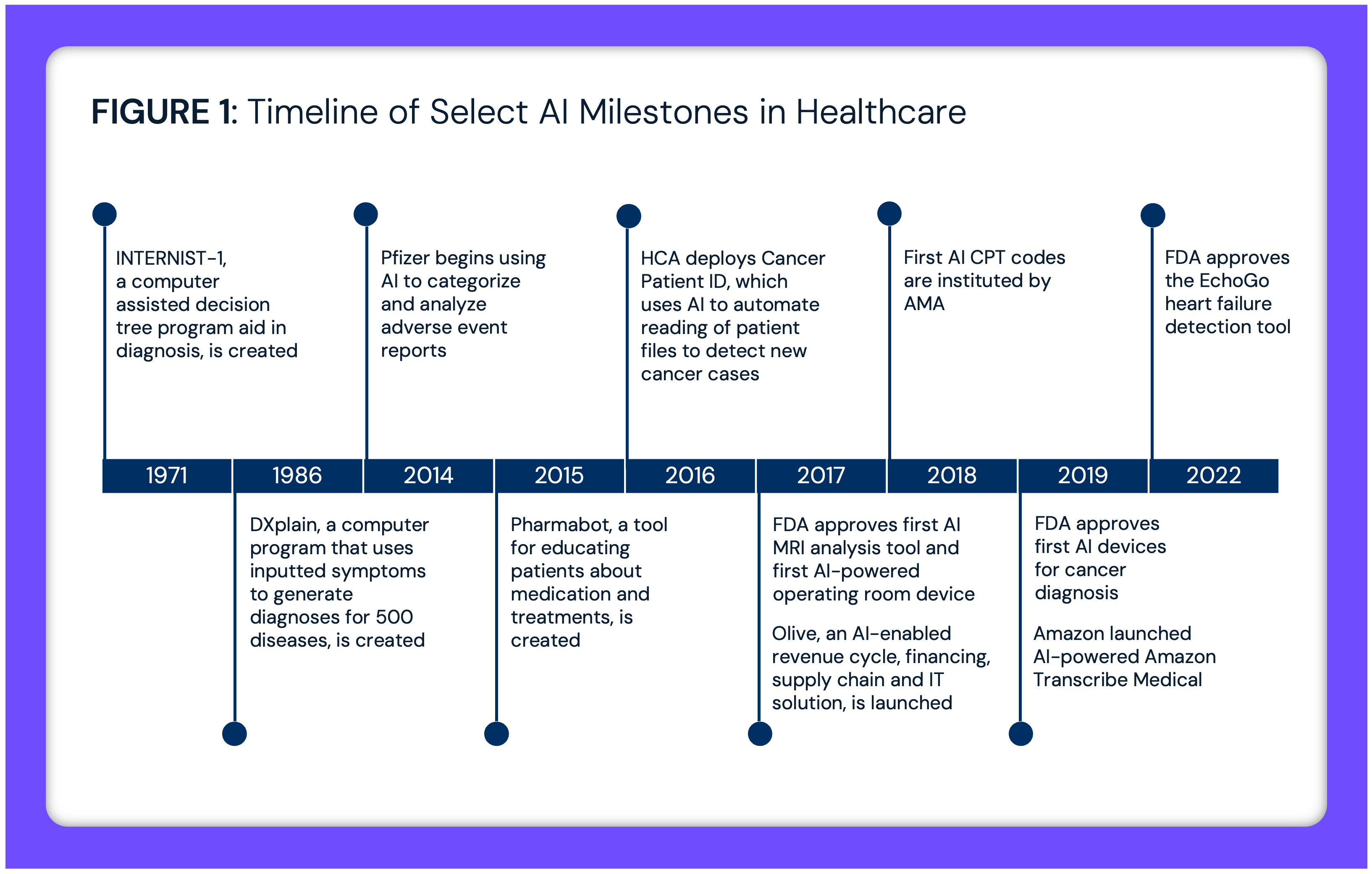
Trends in attention deficit/hyperactivity disorder (ADHD) diagnosis and treatment have evolved in recent years, shaped by regulatory flexibilities issued during the COVID-19 pandemic, expanded use of telehealth for behavioral health and changing prescribing patterns. Millions of American children and adults have been diagnosed with ADHD, and demand for stimulant medications has continued to increase despite shortages and increased regulatory scrutiny. A recent catalyst is the pandemic-driven acceleration of virtual care utilization, which has resulted in unprecedented growth in e-prescribing from digital health platforms specializing in ADHD treatment.
Background
ADHD affects an estimated 7M U.S. children and adolescents ages 3 to 17 — roughly 11.4% of this population.1 Previous research has shown that aggregate ADHD patient volume has consistently increased since Q1 2019, except for a decline in Q2 2020 corresponding with the onset of the COVID-19 pandemic.2 Our research has also found that overall stimulant prescriptions have increased significantly since the COVID-19 pandemic, particularly among adults under age 45.3 This increase occurred despite nationwide shortages of stimulant medications that began in October 2022 and have continued into 2025, affecting patient access and treatment continuity.4,5
The growth in ADHD patient volume and stimulant prescribing coincided with the COVID-era adoption of telehealth services for behavioral health conditions, with e-prescribing of stimulants increasing over 30X from 2019 to 2023.6 This shift resulted from Drug Enforcement Administration (DEA) guidance during the pandemic that allowed remote prescribing of controlled substances. The pandemic-era waiver for prescribing Schedule II through Schedule V medications via telehealth was extended several times and is set to expire December 31, 2025.
Researchers have concluded that while telehealth poses significant opportunities for the diagnosis of ADHD, more evidence is required to determine the effects of long-term digital treatment and monitoring of ADHD.7 The expansion of telehealth and e-prescribing spawned numerous digital health platforms that specifically targeted adult ADHD diagnosis and treatment, many of which utilized direct-to-consumer (DTC) marketing strategies and subscription-based models. Stimulant medications for ADHD symptom management present unique prescribing considerations due to their classification as Schedule II controlled substances. The DEA and FDA have expressed concerns about diversion and misuse, as well as prescription practices that deviate from clinical guidelines, particularly within digital health platforms, prompting legal action against DTC providers like Cerebral and Done.8,9.
Stimulant prescribing — both traditional and virtual — has increased disproportionately to ADHD disease burden that is evident in traditional medical claims data, warranting further examination of ADHD treatment and prescribing patterns.
Analytic Approach
National all-payer claims data from 2018 to 2023 were analyzed to assess ADHD patient volume and stimulant prescribing. Results were segmented by sex and age. For ADHD patients, the most common comorbid behavioral health conditions were examined. To examine diagnosis history, among patients with a stimulant prescription between 2018 and 2023, the presence of an ADHD diagnosis within 365 days of the prescription date was assessed. Additionally, the dosages of prescribed stimulants were analyzed over time.
Findings
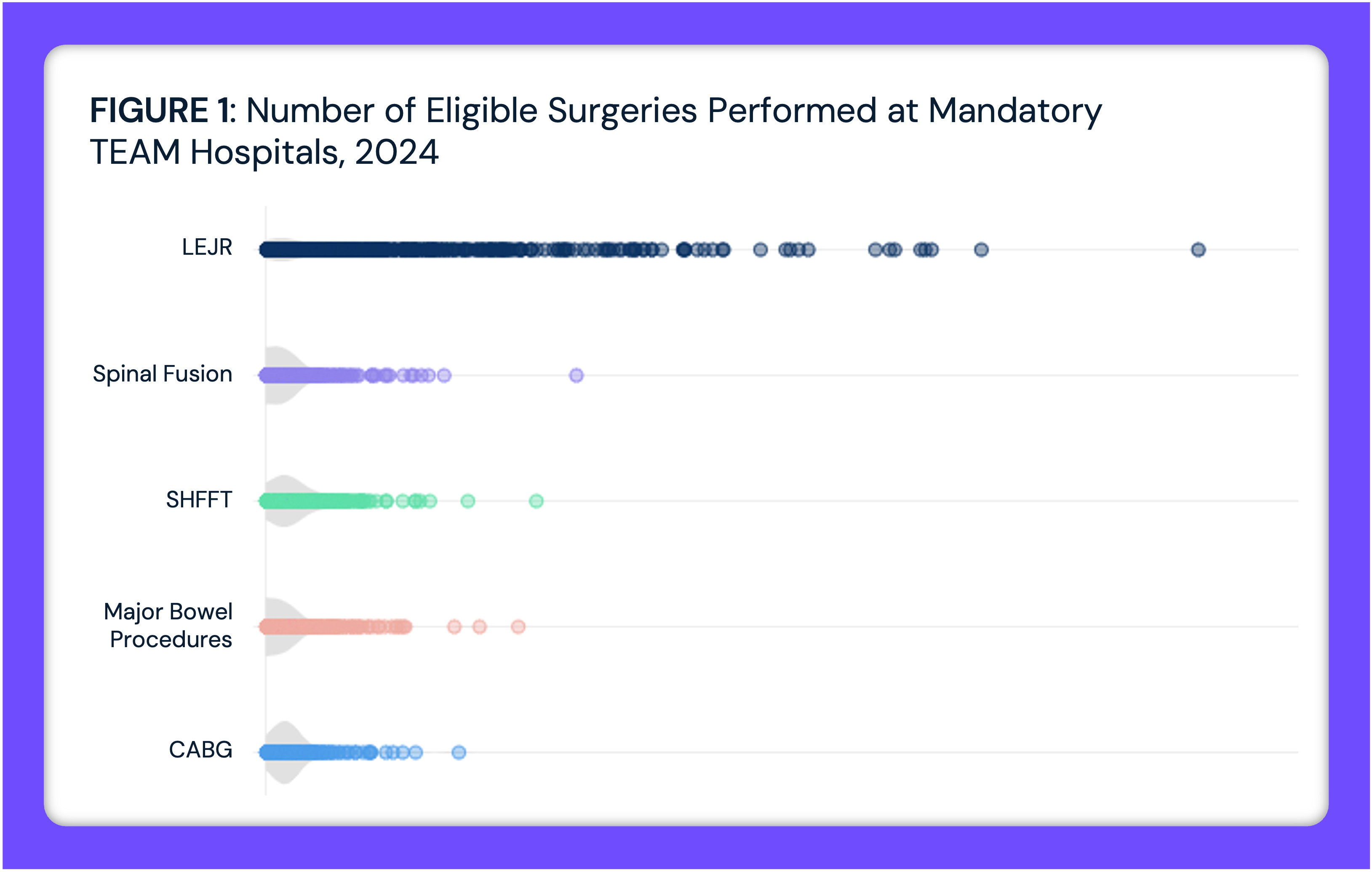
From 2018 to 2023, ADHD patient volume trends varied substantially by age and sex. While ADHD patient volume among children and adolescents (ages 0-17) declined relative to 2018, particularly among males, adult ADHD diagnoses (ages 18-49) saw a substantial increase, with the most pronounced growth among females, increasing by 61.7% from 2018 to 2023 (Figure 1). Older adults (ages 50+) also showed steady year-over-year increases, with a 45.6% overall increase in ADHD patient volume during the time period.
📌 The graph below is interactive. Hover over the point(s) for more information.
ADHD is frequently comorbid with a range of behavioral health conditions. Other anxiety disorders are the most common comorbidity, affecting 33.1% of ADHD patients, followed by recurrent major depressive disorder (19.5%) and adjustment disorders linked to severe stress (19.4%) (Figure 2). Depressive episodes (11.7%) and bipolar disorder (8.4%) are also frequent comorbidities for ADHD patients. The presence of substance use disorders, such as alcohol-related (3.4%) and opioid-related disorders (4.5%), suggests potential challenges in long-term treatment adherence and underscores the importance of integrated behavioral health interventions in ADHD management.
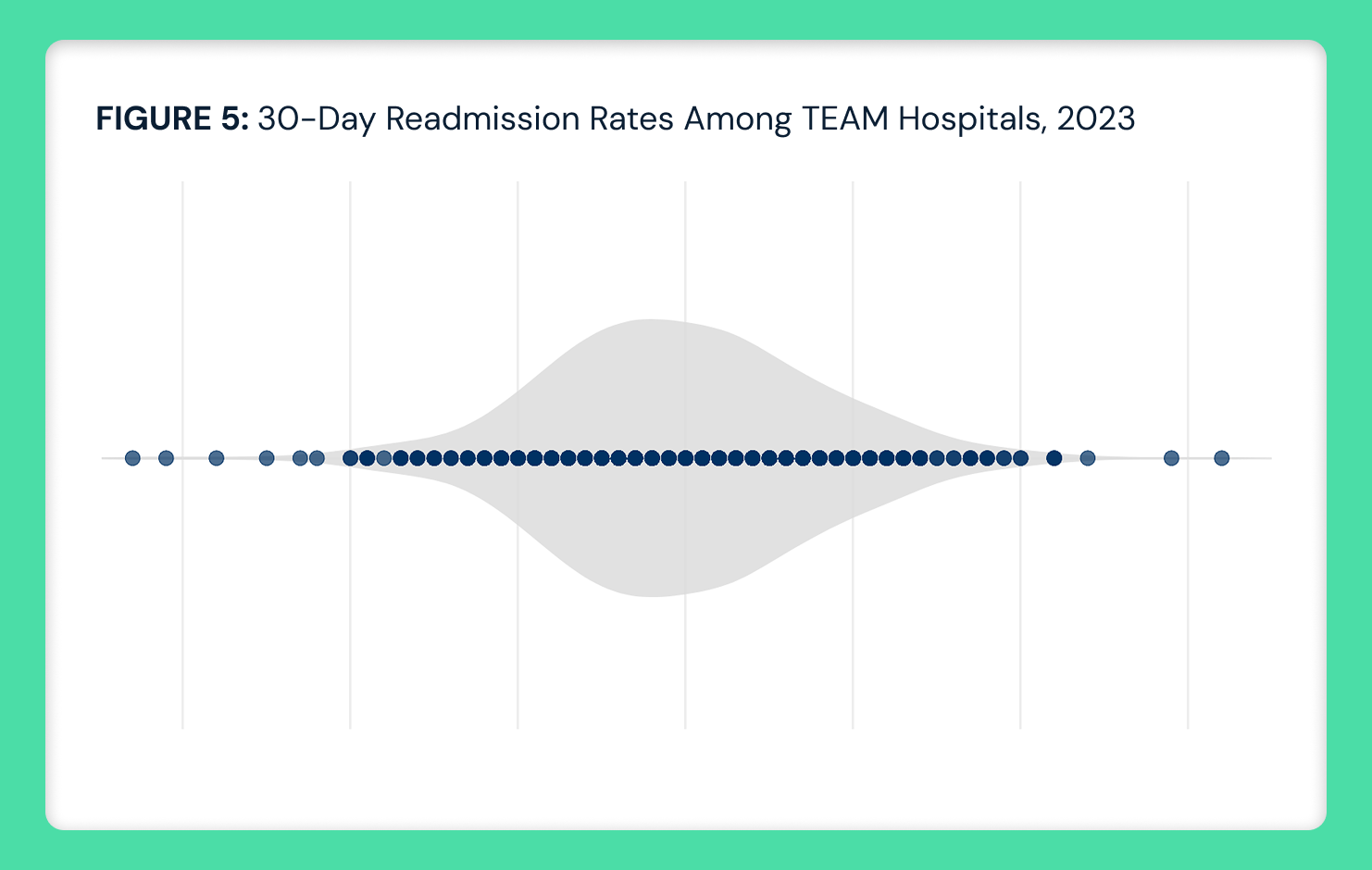
 Since 2019, an increasing proportion of patients prescribed stimulants do not have a documented ADHD diagnosis. In 2018, 86.4% of stimulant recipients had an ADHD diagnosis in their medical claims, but by 2023, this percentage had dropped to 57.0% (Figure 3). Conversely, the proportion of stimulant patients without an ADHD history rose from 13.6% in 2018 to 43.0% in 2023, with the most pronounced increases occurring after 2020. These trends likely reflect expanded use for off-label indications and increased prescribing through digital health platforms.
Since 2019, an increasing proportion of patients prescribed stimulants do not have a documented ADHD diagnosis. In 2018, 86.4% of stimulant recipients had an ADHD diagnosis in their medical claims, but by 2023, this percentage had dropped to 57.0% (Figure 3). Conversely, the proportion of stimulant patients without an ADHD history rose from 13.6% in 2018 to 43.0% in 2023, with the most pronounced increases occurring after 2020. These trends likely reflect expanded use for off-label indications and increased prescribing through digital health platforms. The distribution of prescribed stimulant dosages has shifted notably from 2018 to 2023 with respect to lower- and higher-dose prescriptions. Prescriptions in the 5-10 mg dosage range consistently represented the largest share but declined from 40.9% in 2020 to 34.7% in 2023 (Figure 4). While mid-range dosages (10-20 mg) remained relatively stable, the highest dosages (60-70 mg) gradually declined over the study period, with 70 mg prescriptions decreasing from 6.3% in 2018 to 4.3% in 2023. The increased proportion of low-dosage stimulant prescriptions could reflect the growing number of mild or self-perceived ADHD symptoms seeking treatment.
The distribution of prescribed stimulant dosages has shifted notably from 2018 to 2023 with respect to lower- and higher-dose prescriptions. Prescriptions in the 5-10 mg dosage range consistently represented the largest share but declined from 40.9% in 2020 to 34.7% in 2023 (Figure 4). While mid-range dosages (10-20 mg) remained relatively stable, the highest dosages (60-70 mg) gradually declined over the study period, with 70 mg prescriptions decreasing from 6.3% in 2018 to 4.3% in 2023. The increased proportion of low-dosage stimulant prescriptions could reflect the growing number of mild or self-perceived ADHD symptoms seeking treatment.
📌 The graph below is interactive. Hover over the bar(s) for more information.
Conclusion
The emergence of DTC mental health platforms coincided with significantly increased e-prescribing rates of stimulants, particularly among young adults, despite ongoing stimulant shortages and heightened regulatory scrutiny. Generally, this trend may call into question the concept of “healthcare consumerism,” particularly pharmaceutical therapies. More specifically, this trend raises concerns about potential health risks associated with off-label stimulant use, including cardiovascular effects, dependence and misuse, particularly among individuals without a clinically established need. The presence among ADHD patients of comorbid behavioral health conditions, such as anxiety, mood disorders and substance use disorders, further underscores the importance of careful prescribing and monitoring practices.
In contrast, the anticipated surge in adolescent ADHD diagnoses and treatment during the pandemic did not materialize. Given that ADHD symptoms are often first identified in structured classroom settings by teachers and counselors, the decline suggests that school closures and limited in-person interactions may have delayed diagnoses and subsequent treatment initiation. At the same time, the pandemic saw a surge in adult ADHD diagnoses, driven in part by DTC marketing and increase in behavioral health diagnosing. This shift raises the possibility that rather than being entirely ‘missed,’ some of these diagnoses were instead actively sought out by adults who had long experienced symptoms but remained undiagnosed.
One of the many questions about America’s pandemic response is whether it revealed a previously undiagnosed volume of behavioral health issues in the American public or instead catalyzed a transformation in ADHD diagnosis and treatment – or both. Without question, traditional behavioral health care pathways were disrupted by the pandemic response, resulting in broad telehealth expansion and regulatory waivers for remote prescribing. What is not yet known is whether the data about an increase in prescribing behavioral health medications reflects correlation or causation to the pandemic response.
As the expiration of pandemic-era prescribing flexibilities approaches in December 2025, the future of stimulant prescribing and ADHD treatment more broadly remains uncertain. A shift toward stricter regulation, such as reinstating in-person evaluation requirements or increasing oversight of digital prescribing, could curb the widespread accessibility of stimulant medications, potentially reducing misuse while also creating new barriers for patients with clinical needs.
The long-term implications of these changes warrant significant investigation. While telehealth introduced immediate access to care, particularly for adults seeking ADHD treatment, it has also introduced risks related to prescribing oversight, clinical appropriateness and patient safety. Moving forward, policymakers and healthcare providers must balance accessibility with responsible prescribing practices to ensure that digital ADHD treatment models support both clinical efficacy and patient safety. The patterns observed in ADHD prescribing may serve as a broader indicator of how regulatory shifts will shape digital behavioral health treatment across multiple conditions in the coming years.
- Studies






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)