Research
Antibiotic Overprescribing Remains High in Certain Provider Types, Care Settings and Regions
July 28, 2025Study Takeaways
- Allied health providers demonstrated higher low-value antibiotic prescribing rates than physicians, averaging 14.6% vs. 11.9%.
- Emergency departments consistently had the lowest rate of antibiotic overprescribing, averaging 5.7%, while telehealth and urgent care exhibited higher rates at 15.5% and 15.2%, respectively.
- In 2023, low-value antibiotic prescribing rates varied widely by state, ranging from 7.3% in Wisconsin to 22.8% in Arkansas.
Antibiotic overprescribing is a persistent public health challenge with significant implications for treatment efficacy and patient safety. Consistent with the analysis of low-value duplicate imaging in the 2024 Trends Shaping the Health Economy Report, the inappropriate and excessive use of antibiotics also contributes to escalating healthcare costs.1 Additionally, overprescribing exacerbates the growing global health threat of antibiotic-resistant infections.
Background
Unnecessary antibiotic prescriptions are a hallmark of low-value healthcare utilization.2 In 2022, U.S. community pharmacies dispensed 236.4M antibiotic prescriptions, equivalent to approximately seven prescriptions for every 10 people in the outpatient setting. Notably, the Centers for Disease Control and Prevention (CDC) estimates that at least 28% of outpatient antibiotic prescriptions in the U.S. are not clinically necessary, presenting an important opportunity for resource optimization and improved stewardship.3
Prescribing behaviors are influenced by multiple factors, including clinical training, financial incentives, patient expectations, time constraints and organization-specific policies and protocols. The economic burden of unnecessary antibiotic prescribing extends beyond direct medication costs. Overuse increases healthcare expenditures through adverse drug reactions, secondary infections and the long-term consequences of antimicrobial resistance — estimated to drive $4B to $5B in annual healthcare spending.4
This study examines variation in antibiotic prescribing patterns across provider types, care settings and geographic regions, offering insights for health economy stakeholders seeking to enhance antibiotic stewardship efforts.
Analytic Approach
National all-payer claims data were analyzed to assess low-value antibiotic prescribing practices across care settings from 2018 to 2023. Visits for viral upper respiratory infections, which do not warrant antibiotic treatment, were identified and isolated as an index event. We then examined antibiotic prescriptions written by the same provider on the same day as the initial visit. Antibiotic prescribing was examined across provider types, including physicians and allied health providers, multiple care settings, including telehealth, urgent care, physician offices and emergency departments, and by state. For each analysis, the total number of visits with applicable diagnosis codes was calculated, along with the number of visits resulting in antibiotic prescriptions and the proportion of visits leading to antibiotic treatment.
Findings
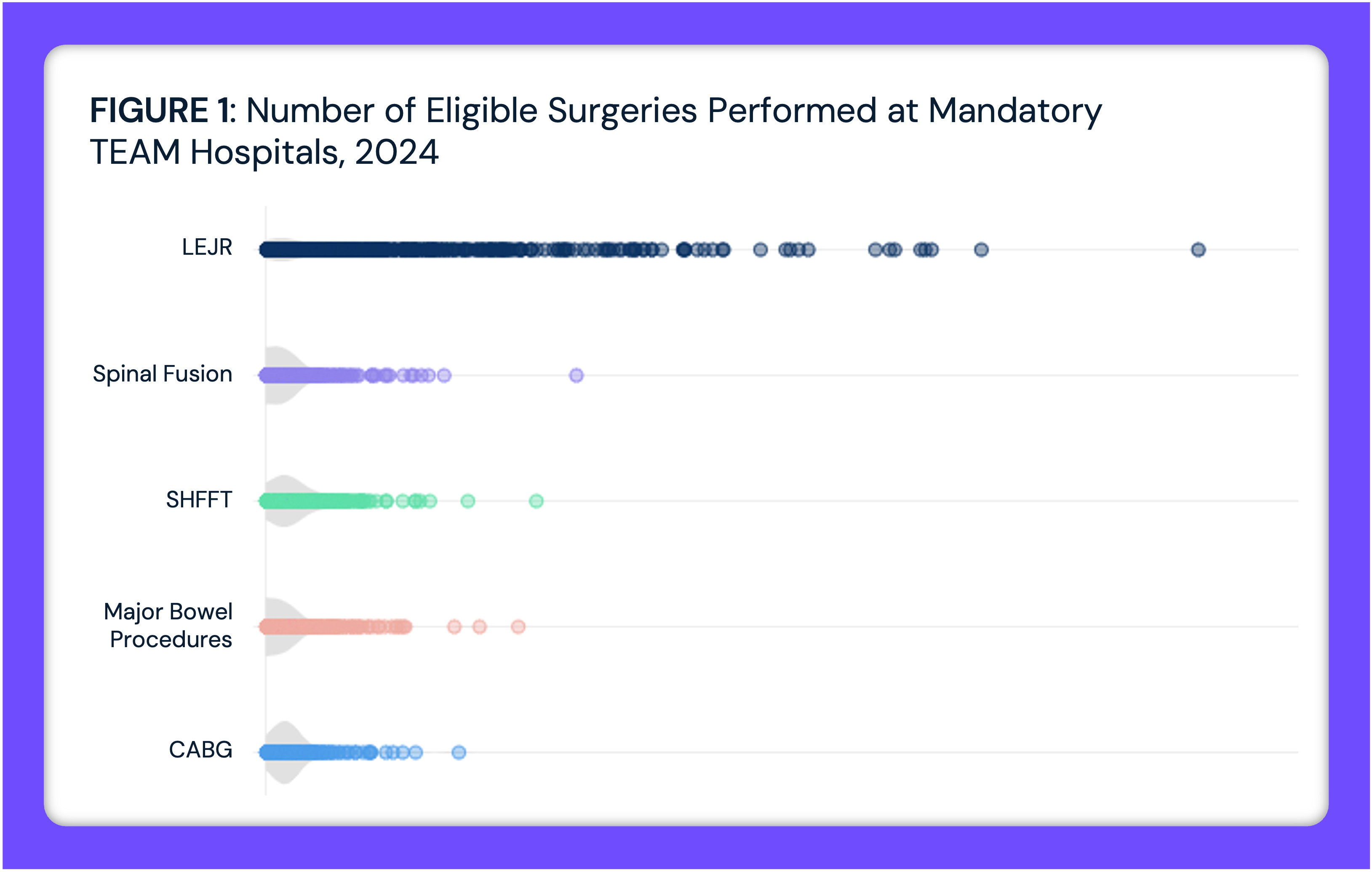
Rates of unnecessary, or low-value, antibiotic prescribing varied across provider types, across years. Allied health providers — nurse practitioners (NPs) and physician assistants (PAs) — consistently prescribed antibiotics for upper respiratory infections at higher rates than physicians, averaging 14.6% vs. 11.9% (Figure 1). An increase was observed across all provider types in 2023, with rates reaching 17.1% for NPs/PAs, 13.7% for physicians and 15.0% for other providers — the highest levels observed during the study period. Variation in antibiotic prescribing for upper respiratory infections was also observed across care settings from 2018 to 2023. Emergency departments consistently maintained the lowest prescribing rates, averaging 5.7%, while telehealth and urgent care demonstrated notably higher rates at 15.5% and 15.2%, respectively (Figure 2). An increase was observed in 2023, with urgent care reaching 17.4%, telehealth 17.0%, physician offices 15.7% and emergency departments 6.9%.
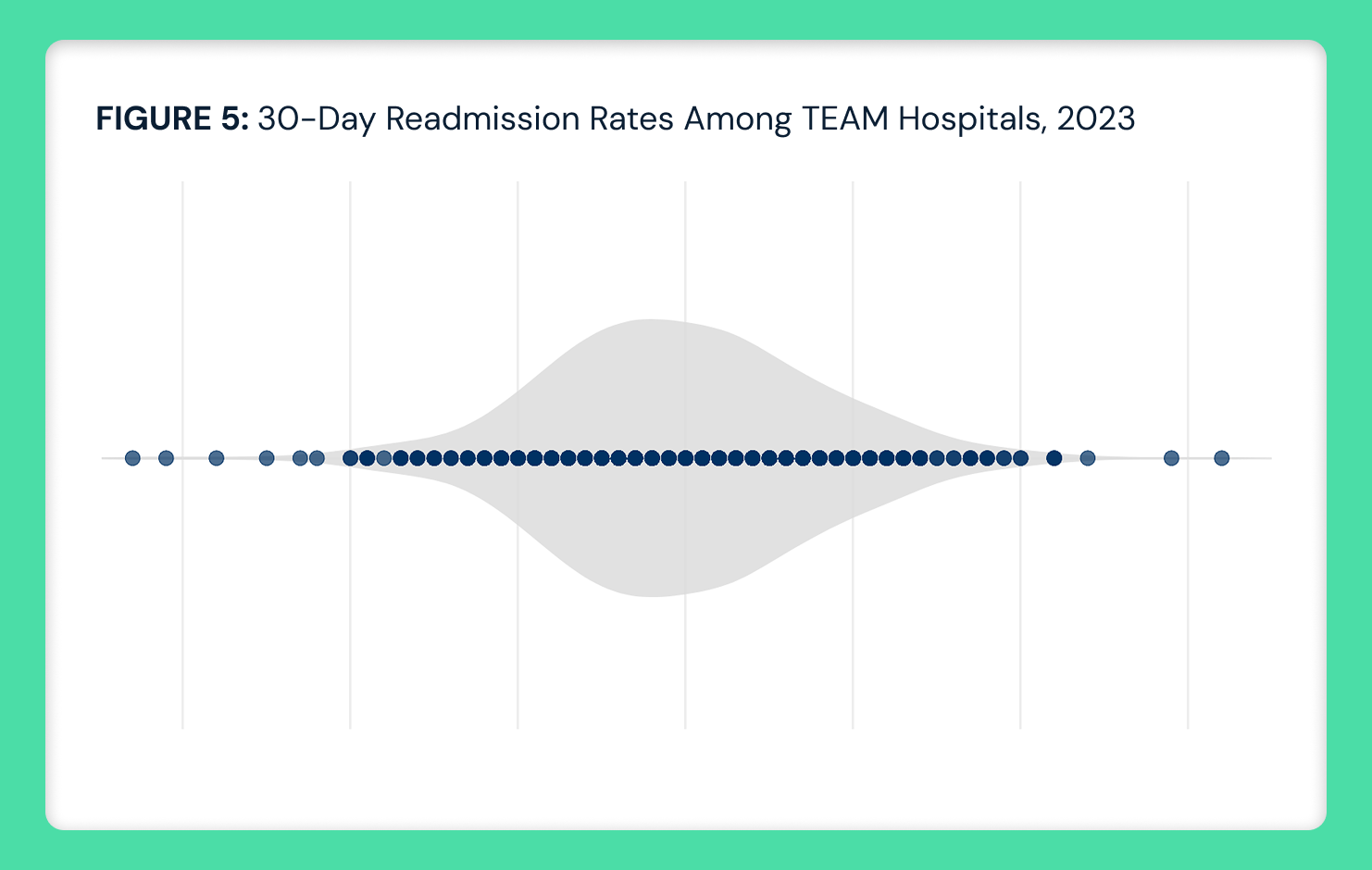
Variation in antibiotic prescribing for upper respiratory infections was also observed across care settings from 2018 to 2023. Emergency departments consistently maintained the lowest prescribing rates, averaging 5.7%, while telehealth and urgent care demonstrated notably higher rates at 15.5% and 15.2%, respectively (Figure 2). An increase was observed in 2023, with urgent care reaching 17.4%, telehealth 17.0%, physician offices 15.7% and emergency departments 6.9%. In 2023, antibiotic prescribing for upper respiratory infections patterns reveal substantial geographic variation. Prescribing rates ranged from a low of 7.3% (Wisconsin) to a high of 22.8% in (Arkansas) (Figure 3). The state median rate of low-value prescriptions was 13.3%, and the percentage of low-value prescriptions ranged between 11% to 16% in most states. However, several states in the Southeast demonstrated notably higher prescribing rates, including Arkansas (22.8%), Alabama (21.9%) and Kentucky (18.0%).
In 2023, antibiotic prescribing for upper respiratory infections patterns reveal substantial geographic variation. Prescribing rates ranged from a low of 7.3% (Wisconsin) to a high of 22.8% in (Arkansas) (Figure 3). The state median rate of low-value prescriptions was 13.3%, and the percentage of low-value prescriptions ranged between 11% to 16% in most states. However, several states in the Southeast demonstrated notably higher prescribing rates, including Arkansas (22.8%), Alabama (21.9%) and Kentucky (18.0%).
📌 The graph below in interactive. Hover over a state for more information.
Conclusion
The wide variation in antibiotic prescribing for upper respiratory infections practices across provider types, care settings and states is yet another opportunity to optimize resource allocation and costs in the health economy. Notably, this overuse persists despite extensive emphasis on antibiotic prescribing stewardship, which suggests even more profound challenges in reducing the amount of other low-value care with comparatively less attention. With unnecessary antibiotics contributing an estimated $4B-$5B in annual healthcare spending, the observed prescribing patterns — particularly the elevated prescribing rates for upper respiratory infections, which generally do not warrant antibiotic prescriptions — underscore the need to improve and align treatment patterns with evidence-based guidelines. Additionally, the growth of direct-to-consumer and virtual care providers has enabled more e-prescribing of antibiotics.
The persistent variation, occurring even with existing stewardship efforts, raises critical questions about the broader landscape of unnecessary medical interventions and the barriers to de-adoption and implementation of evidence-based care. What is the root cause of prescribing medications without clinical indication? What interventions, like provider education and modified care protocols, will lead to more appropriate prescribing behavior? How can health systems better align prescribing practices across different care settings while maintaining appropriate clinical autonomy? What changes to benefit design might reduce the “fill rates” of unnecessary prescriptions? Why haven’t workflows embedded in electronic medical record systems reduced the percentage of unnecessary prescriptions? Eliminating low-value care is the “low hanging fruit” of trying to bend the cost curve in the health economy, and every stakeholder has a part to play.
- Studies






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)