Studies Archive
Delayed Care Materializing in Greater Healthcare Costs…and Patient Acuity
August 7, 2022In last week’s edition of The Compass, we explored how care delays, changing benefit design, and inflation will likely result in premium hikes and more expensive healthcare for the average American.1 To extend this analysis, we examined changes in healthcare use by care setting to explore if delayed care has begun to manifest in increased patient acuity.
Background
Our research has demonstrated that consumers have been slow to return to primary care and, in tandem, recommended preventive screenings.2,3,4 Underuse of high-value services is generally expected to result in increased morbidity and mortality. Beyond the population-level health consequences, a sicker population will be more expensive to manage. Rather than preventing chronic disease or diagnosing acute illnesses in a more timely manner, a sicker population will require more frequent, costly, and intensive services. While patient acuity is often categorized by the severity of specific conditions and diagnoses, settings and types of care can serve as a broad indicator for higher patient acuity (e.g., higher inpatient volumes and lower preventive care volumes).
Analytic Approach
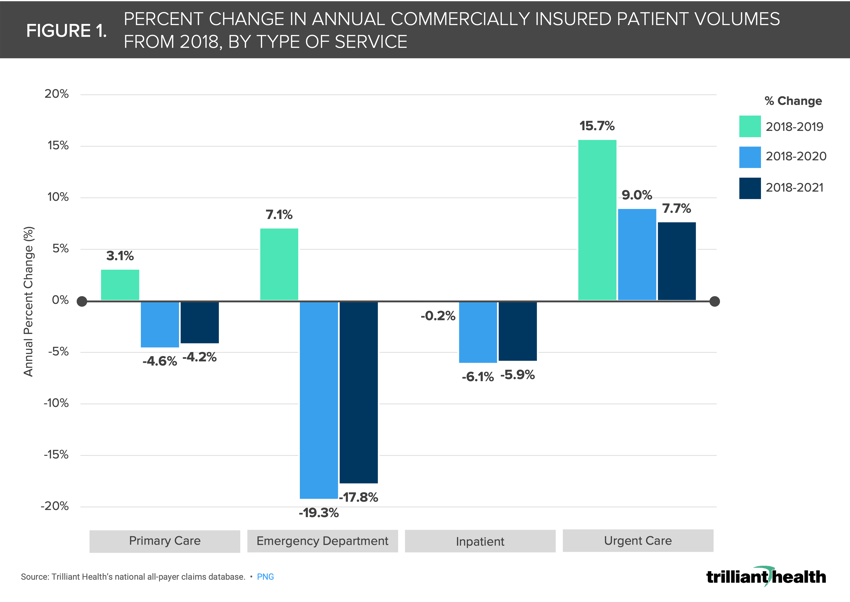
To better understand trends in patient acuity, we compared commercial annual patient volumes from 2019-2021 to 2018 by care setting: primary care, emergency department, urgent care, and inpatient. For a more accurate comparison of preventive care utilization, we excluded encounters involving treatment, testing, and vaccination for COVID-19.
Findings
The ideal care pathway for patients begins with preventive care (i.e., receiving timely recommended screenings and an annual visit with an established primary care physician). Across all age groups, females have a higher mean number of primary care office visits (1.47) per year than males (1.24).5 While recommendations for screenings and annual wellness visits vary by age and individual risk factors, the Affordable Care Act ensures recommended preventive services are covered at no cost to insured individuals.6
Even so, we find that non-COVID-19 related primary care volumes have steadily decreased, dropping by 14.2% between 2018 and 2021 (Figure 1). Similarly, there have been steady declines in inpatient (-5.9%) and emergency department use (-17.8%) since the onset of the pandemic. In contrast, urgent care patient volumes have increased consistently, up 7.7% in 2021 vs 2018. Taken together, these trends suggest that some proportion of care was diverted from primary care offices and emergency departments to urgent care settings. Given the consistently declining volumes and delay of care across care settings (excluding urgent care), these data suggest that worsening patient acuity for the commercially insured has not yet materialized through growing inpatient volumes.
 Notably, these observed declines have likely not affected all commercially insured patients equally. Disparities within the commercially insured population are often not researched due to gaps in race and ethnicity data, particularly in the employer-sponsored commercial population. However, a recent study by Morgan Health and NORC revealed substantial health disparities in the employer-sponsored population regarding chronic conditions, maternal health, behavioral health, substance use, and access to care. Notably, patients of racial/ethnic minority backgrounds experienced more barriers to accessing care. Specifically, Black patients were 4.9 percentage points more likely than White patients to have visited an emergency department.7
Notably, these observed declines have likely not affected all commercially insured patients equally. Disparities within the commercially insured population are often not researched due to gaps in race and ethnicity data, particularly in the employer-sponsored commercial population. However, a recent study by Morgan Health and NORC revealed substantial health disparities in the employer-sponsored population regarding chronic conditions, maternal health, behavioral health, substance use, and access to care. Notably, patients of racial/ethnic minority backgrounds experienced more barriers to accessing care. Specifically, Black patients were 4.9 percentage points more likely than White patients to have visited an emergency department.7
While analyzing shifts in utilization by care setting is just one indicator of patient acuity, it is an important signal for what it is to come. Our prior research showed that before the pandemic, cardiovascular utilization for younger adults (ages 25-44) was projected to grow in certain major CBSAs primarily due to population trends (e.g., migration). However, with the pandemic factored in, that growth is instead primarily driven by evolving needs (e.g., changes in burden of disease).8 Future research is needed to examine the changes in conditions presented among patients.
The sustained decline in commercially insured patient volumes across settings of care raises concern for future morbidity and mortality in this population segment, which has historically been characterized as younger and healthier than Medicare or uninsured populations.9 Notably, this trend predates the pandemic, reiterating the need for healthcare strategies that accurately predict future healthcare trends.10 Providers and payers alike should be considering new ways to incentivize the return to primary care and fill in this observed gap, beyond changes in cost sharing.
Thanks to Kelly Boyce and Katie Patton for their research support.






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)



