Studies Archive
Cancer Screening Rates Following the COVID-19 Pandemic Peak Vary Regionally
January 22, 2023Key Takeaways
-
The rate of breast, cervical, and colorectal cancer screenings fell 40%, 36%, and 45%, respectively, in Q2 2020 compared to pre-pandemic median quarterly levels.
-
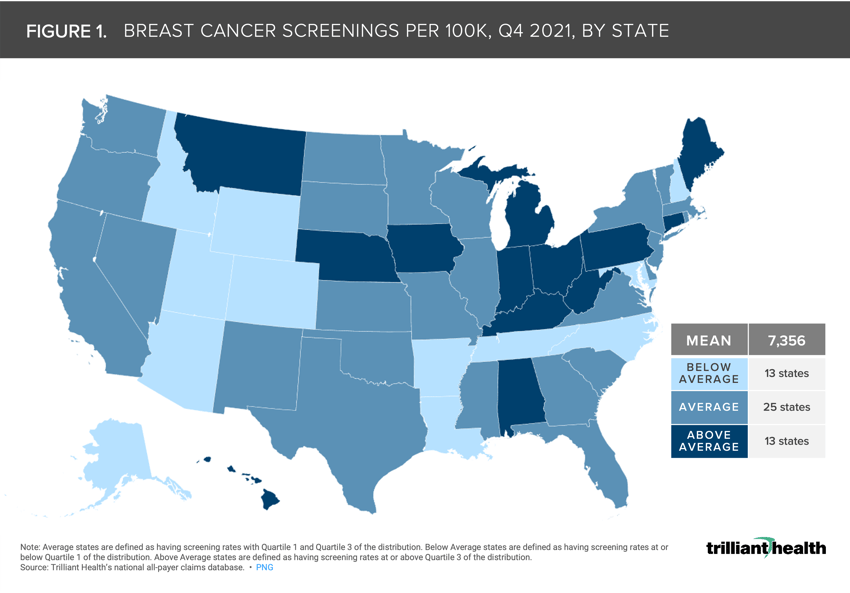
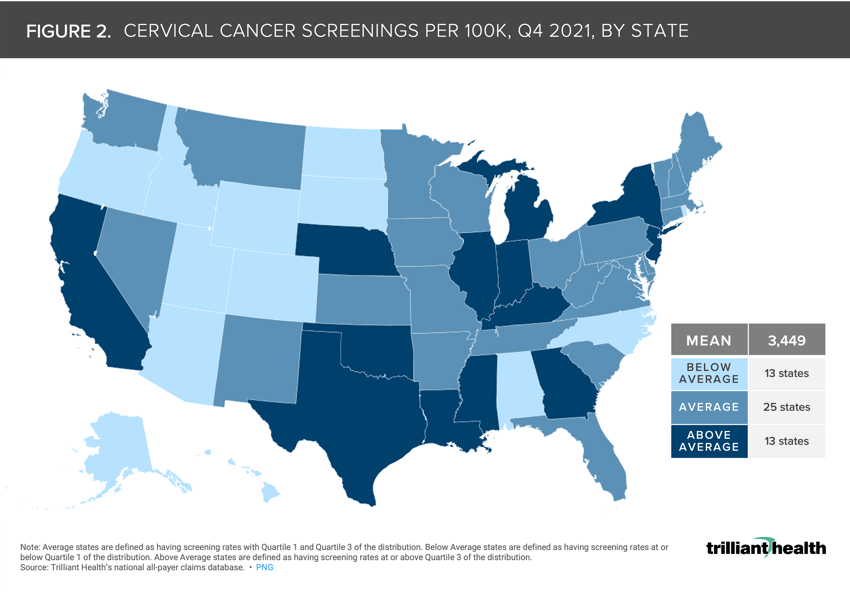
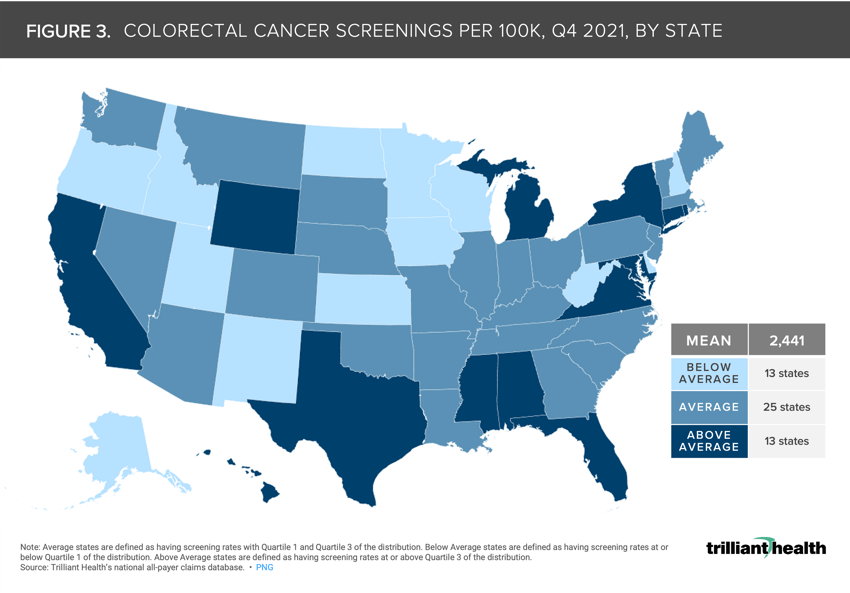
Nationally, the average screening rates for breast, cervical, and colorectal cancers in Q4 2021 were 7,356, 3,449, and 2,441 per 100K, respectively.
-
States characterized by low cancer screening rates also saw a net decline in its physician workforce from 2019 to 2022.
This past November, my Trilliant Health colleagues and I published a research letter in JAMA Oncology titled Rates of Routine Cancer Screening and Diagnosis Before vs After the COVID-19 Pandemic. Our findings suggest that screening rates for breast, cervical, and colorectal cancer rebounded after the initial stages of the pandemic; however, analysis of a longer timeframe reveals a decline in preventive cancer screening compared to 2019 levels. Because healthcare is local, we wanted to understand whether this trend varied by geography and, if so, what factors might explain regional variation in cancer screening?
Background
According to our research, while breast cancer screening mammography decreased by 40% in Q2 2020 compared to a pre-pandemic quarterly rate, screening mammography rebounded to pre-pandemic levels in the second half of 2020, only to decline again in 2021, with quarterly deficits ranging from 6% to 17%. Cervical cancer screening rates fell 36%, from a pre-pandemic quarterly rate of 5,602 to 3,563 per 100K in Q2 of 2020, while colorectal cancer screening declined 45% from a pre-pandemic quarterly average rate of 3,162 to 1,746 per 100K over the same timeframe.
A recent study from the American Cancer Society (ACS) found that U.S. cancer death rates declined by 33% between 1991 and 2020, equating to 3.8M avoided cancer-related deaths.1 Despite this progress, the ACS researchers raise concerns about the rising incidence of breast, prostate, and uterine cancer in recent years, which seems likely to continue as fewer screenings were conducted during 2020 and 2021.
Analytic Approach
To determine the extent to which Americans delayed cancer screenings over the past three years, we examined cancer screenings recommended by the U.S. Preventive Services Task Force for certain adult populations across payer types (e.g., Medicare, Medicaid, commercial) for the following cancers: colorectal, breast, and cervical. Patients aged 21 to 85 years were included (guideline-concordant target populations for the included screening procedures). For breast and cervical cancer, only women were included.
For this patient cohort, we calculated the annual utilization rate of the recommended screening types (e.g., colonoscopy, blood-based screenings, and stool-based screenings for colorectal cancer) for each distinct cancer in Q4 2021 in all 50 states and D.C. Screening rates were characterized as “Below Average,” “Average,” and “Above Average.” Average states are defined as having screening rates within Quartile 1 and Quartile 3 of the screening rate distribution. Below Average states are defined as having screening rates at or below Quartile 1 of the distribution. Above Average states are defined as having screening rates at or above Quartile 3 of the distribution.
Findings
Nationally, the average screening rates per 100K for breast, cervical, and colorectal cancers in Q4 2021 were 7,356 (Figure 1), 3,449 (Figure 2), and 2,441 (Figure 3), respectively. Alaska, Idaho, and Utah are the only three states with below-average screening rates across each cancer type, whereas Michigan was the only state with above-average screening rates throughout the timeframe. Screening rates in Massachusetts, Missouri, Nevada, South Carolina, Vermont, and Washington were considered average across all cancer types. While screening rates for breast and cervical cancer screening were considered below average in Wyoming, screening rates for colorectal cancer were above average in Q4 2021.
The observed regional variation could be attributed to provider availability, intentional avoidance of medical care (e.g., COVID-19 fear, rising healthcare costs, and growing provider mistrust), and awareness of recommended screenings. For example, the states where screening rates were below average across cancer types (AK, ID, UT) also saw a net decline in physician workforce from 2019 to 2022.2 Conversely, two metropolitan CBSAs in Michigan (Kalamazoo-Portage and Ann Arbor) were among top regions in the U.S. with high a proportion of primary care physicians relative to population size.3
Nationally, screening remained below pre-pandemic levels for the three included cancer types, and screening rates varied across states. The JAMA Oncology study findings suggest that screening quickly rebounded after the initial stages of the pandemic; however, analysis of a longer timeframe reveals a concerning decline in preventive cancer screening. The long-term secular decline in cancer deaths is attributable to improved cancer therapies, not a reduction in the rate of cancer diagnoses. As a result, it is logical to assume that a decline in population-level cancer screenings will ultimately manifest in the diagnosis of at least an equivalent number of cancer cases but at a later stage. To minimize the longer-term morbidity and mortality consequences of this trend, multiple stakeholders will need to develop and implement strategies and tactics to increase guideline-concordant cancer screening from their current levels.
Thanks to Kelly Boyce, Allison Oakes, and Katie Patton for their research support.






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)