Nearly two years into the pandemic, the healthcare delivery system continues to encounter new and persisting challenges. The Omicron variant and healthcare staffing shortage are further exacerbating an already strained system across care settings and regions. Headlines cyclically focus on overwhelmed emergency departments, non-emergent surgery delays, exorbitant urgent care wait times, and inpatient and outpatient department closures. The delineation of appropriate use cases between urgent care centers and emergency departments is well established. Despite guidance encouraging patients not to seek COVID-19 testing at urgent cares or emergency departments, those cases continue to fill waiting rooms across the country.
Medical care that is best suited for a clinic, urgent care, or primary care office has been delayed, deferred, or lost completely at all stages of the pandemic. However, delays in treating non-emergent but chronic medical conditions eventually result in increasing complexity and co-morbidity. As patients seeking treatment for COVID-19 symptoms overwhelm care settings ranging from urgent care centers to emergency departments, it is important to understand whether and where non-COVID-related cases are being treated.
With respect to consumer preference, we know that Willful Endurers are overwhelmingly more likely to utilize urgent care for their primary care needs. The key question is how consumers with different psychographic profiles will respond to an inability to access their preferred care setting. Will they delay care, or seek alternative access points, or forego treatment altogether? For example, are Self Achievers, who are highly motivated about their health and historically unlikely to access urgent care as often (18% compared to 67% of Willful Endurers), increasingly accessing urgent care? If so, what type of care are they seeking?
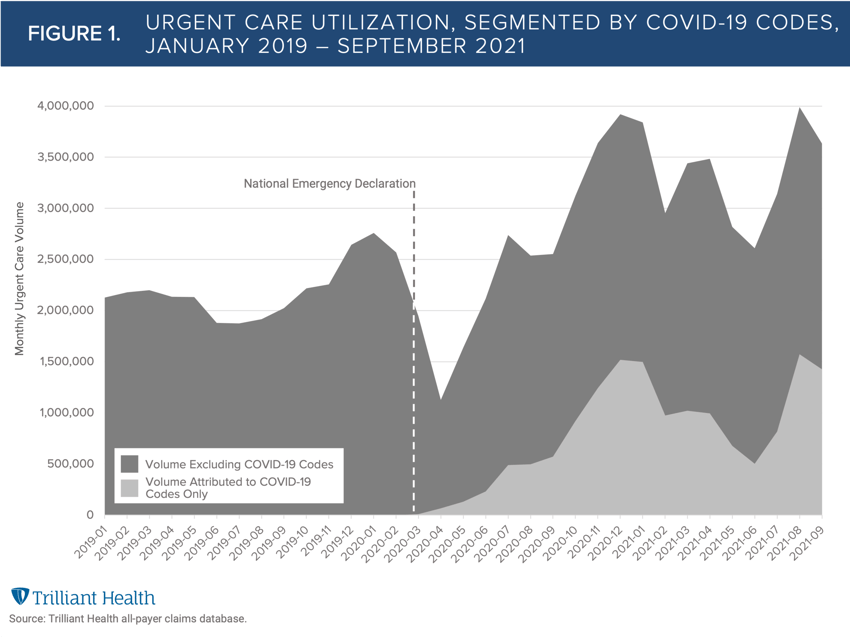
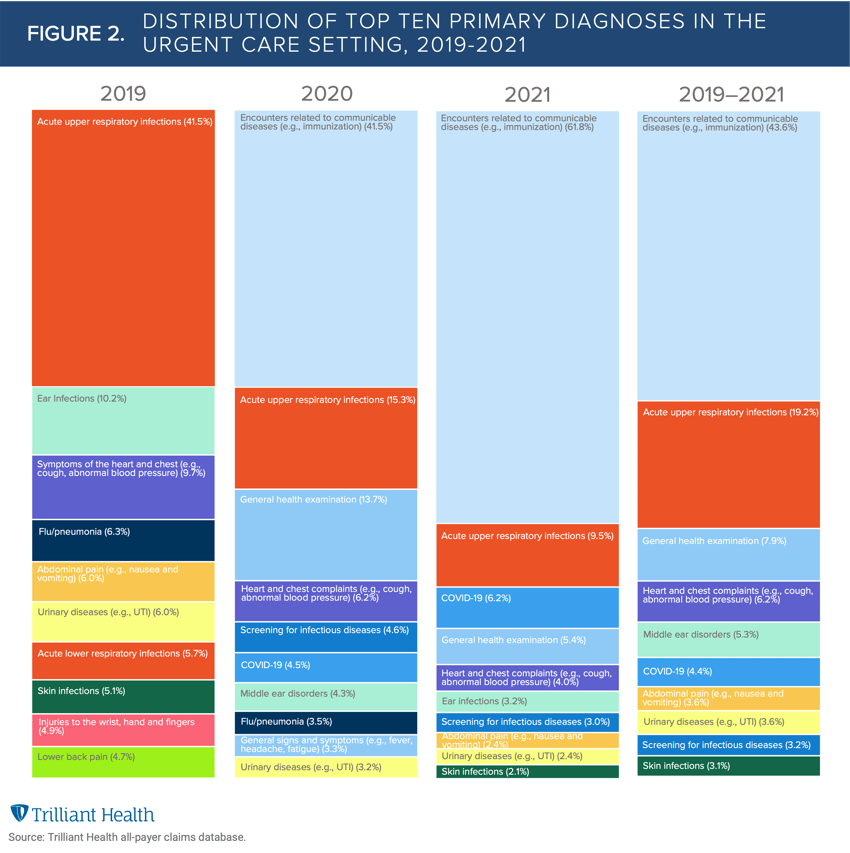
Expanding on last year’s Health Economy Trends Report, we investigated urgent care utilization and the most common primary diagnoses annually since 2019. Although by June 2020 urgent care volumes surpassed pre-pandemic levels, it is evident that urgent care visit volumes are artificially inflated by COVID-19-related visits (e.g., testing, vaccination).
Our analysis reveals that at the onset of the pandemic in March and April 2020, urgent care volumes dropped by 24.2% and 42.1% from the preceding month and were 11.5% and 47.3% lower than volumes in those respective months in 2019 (Figure 1). In contrast, during the spread of the Delta variant in July and August 2021, urgent care volumes increased by 20.3% and 27.1% from the preceding month and were 67.6% and 34.2% higher than volumes in those respective months in 2019. Notably, all of the year-over-year increase is COVID-19-related visits (presenting with symptoms, testing, and vaccination). At the same time, visit types that were characteristic of urgent cares pre-pandemic (e.g., urinary tract infections, ear infections) declined over the same period (Figure 2).
As COVID-19 visits reduce capacity for treatment of primary care and chronic disease, we must consider whether this care is delayed or lost, and the downstream implications of each scenario. Did patients without access to urgent care for non-COVID-19 ailments turn to telehealth? Did they see their primary care provider? Did they opt to go to an emergency department? Did they forego care entirely? Insufficient attention has been paid to analyzing how much basic medical care has been lost during the pandemic and the disease progression for patients whose care needs were initially non-emergent and non-life-threatening. In the coming weeks, we will begin to answer these questions and evaluate the extent to which current clinical acuity is more severe than expected as a result of the reduced availability of primary care services during the pandemic.
Thanks to Kelly Boyce, Katie Patton, and David Taylor for their research support.






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)



