Studies Archive
The Increase in Cost of Care for Patients with Physical and Behavioral Comorbidities Manifests in Different Ways
March 26, 2023Key Takeaways
-
The existence of a behavioral health condition can exacerbate other physical comorbidities (e.g., diabetes), and failure to treat a diagnosed behavioral health condition appropriately can lead to a higher complexity and cost of care.
-
Behavioral health patients with consistent utilization of inpatient and ED settings had higher costs of care (as much as 85.9X higher).
-
The introduction of telehealth was associated with both increases and decreases in total cost of care.
Our 2023 Behavioral Health Trends Report highlighted the fact that untreated behavioral health conditions exacerbate other comorbidities, both in terms of acuity and cost of care. While behavioral health and physical health are intrinsically and empirically linked, the U.S. healthcare system is not well-equipped to address patients’ comorbid physical, behavioral and mental conditions in a coordinated manner.
Background
Research has demonstrated that cost of care is higher for patients with physical and behavioral comorbidities.1 Another study of the Medicare population found that patients with serious mental illness spent substantially more on medical services for the treatment of physical conditions than patients with other common mental health disorders or no known mental illness.
The existence of a behavioral health condition can exacerbate other physical comorbidities (e.g., diabetes), and failure to adequately treat a diagnosed behavioral health condition can lead to higher complexity of care (e.g., frequent emergency department visits). On average, total charge amounts were 20.0% higher for patients that have diabetes, hypertension and depression ($27,511) compared to patients with diabetes and hypertension alone ($22,929).2
Analytic Approach
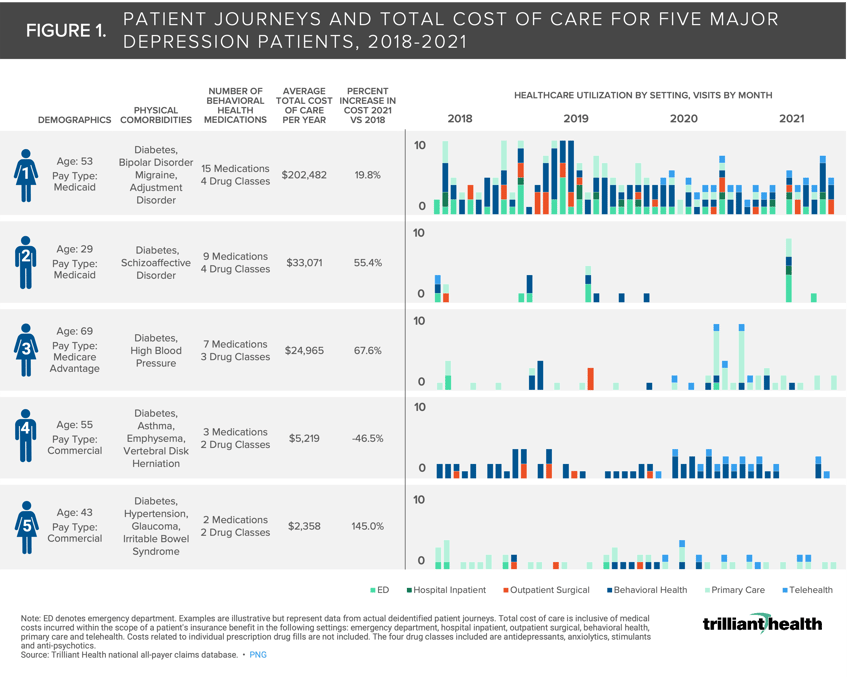
To understand how physical and mental comorbidities manifest in terms of care utilization and total cost, we identified five patients diagnosed with major depression as of 2018 and followed their individual care journeys between 2018 and 2021. All patients were continuously enrolled in health insurance during the study period. The examples are illustrative but represent data from actual deidentified patient journeys across all care settings and provider networks (e.g., health system and CVS Minute Clinic). We classified each patient by age, gender, pay type, physical comorbidities, number of prescribed behavioral health medications, average total cost of care per year and the magnitude change of annual cost of care from 2018 to 2021.
Total cost of care is inclusive of medical costs incurred within the scope of a patient's insurance benefit in the following settings: emergency department, hospital inpatient, outpatient surgical, behavioral health, primary care and telehealth. Costs related to individual prescription drug fills are not included. The four drug classes included are antidepressants, anxiolytics, stimulants and anti-psychotics.
Findings
Patients with consistent utilization of inpatient and ED settings had higher costs of care (85.9X higher for Patient 1 compared to Patient 5 despite similar age and gender) (Figure 1). Notably, the introduction of telehealth was associated with both increases and decreases in total cost of care. Patients 1, 2, 3, and 4 utilized telehealth services in 2020 and 2021, although Patients 1-3 incurred increased costs, while Patient 4 saw a 46.5% decline in total cost of care.
With screenings—and ultimately diagnoses—set to increase given the USPSTF recommendation to screen most adults for anxiety and depression, associated costs are already expected to increase for behavioral health conditions alone.3,4,5 The current supply of behavioral health providers cannot meet this growing demand, so primary care providers are set to take on the responsibility of managing their patients’ physical and mental comorbidities. Improved coordination and integration of physical and mental health are needed to moderate increasing patient costs, which amplify the increasing economic strain on the U.S. healthcare system.
Dive deeper into the findings with Service Line Intelligence | Behavioral Health, a premium subscription that analyzes changes in Behavioral Health demand, supply and yield at the condition, therapeutic, provider and market levels.
Learn More >






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)