Research
Most Behavioral Health Patients, Particularly Those with Alcohol or Substance Use Disorder, Do Not Receive Follow-Up Care After an Emergency Department Visit
Mar 19, 2023 12:01:00 AMKey Takeaways
-
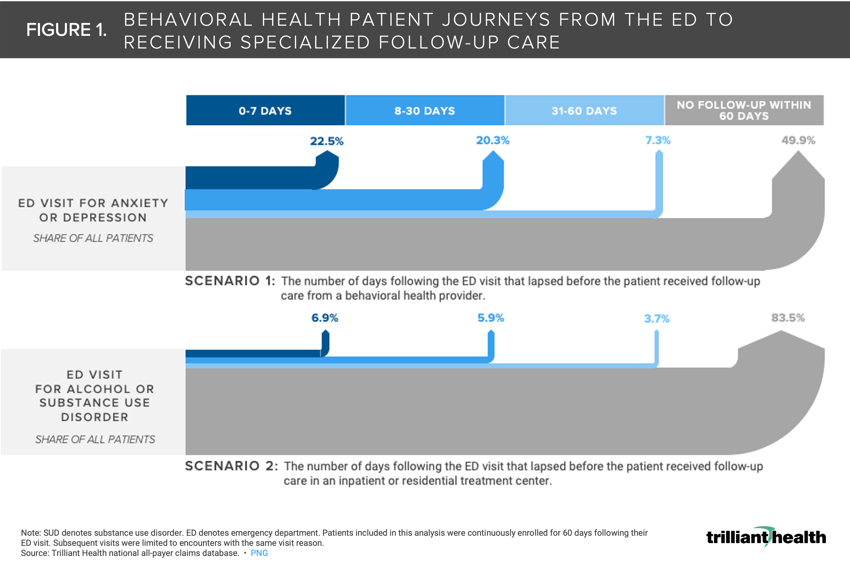
Half of patients who were treated in an emergency department for anxiety or depression did not receive care from a behavioral health provider within 60 days.
-
Over 80% of patients who were treated in an emergency department for an alcohol or substance use disorder did not receive inpatient care within 60 days.
-
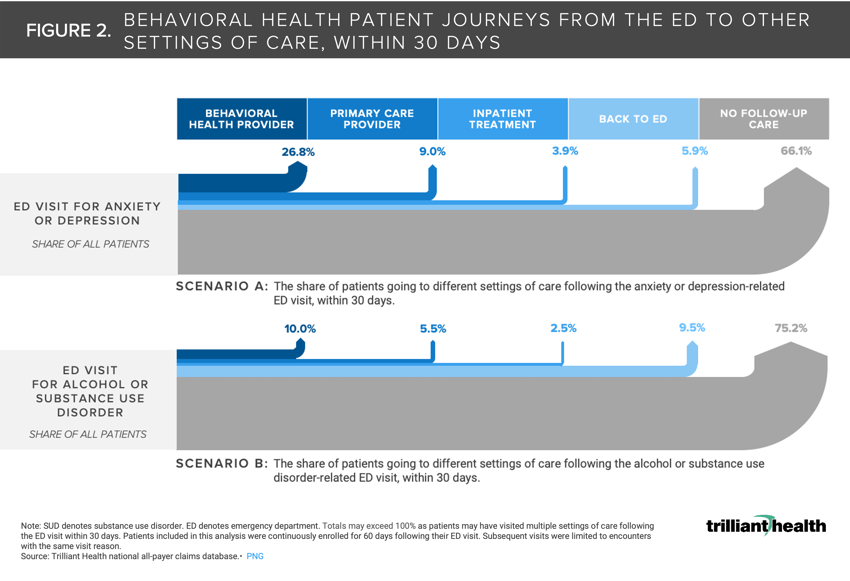
Almost 10% of patients with alcohol or substance use disorder are readmitted in an emergency department within 30 days, as compared to 5.9% of anxiety and depression patients within that timeframe.
Our 2023 Behavioral Health Trends Report highlighted how the most common settings of care where patients receive behavioral health care shifted as a function of the COVID-19 pandemic.1,2 While visits delivered via telehealth increased 45X post-pandemic, fewer visits are taking place in the emergency department (ED) compared to pre-pandemic for a variety of reasons (e.g., fear of contracting COVID-19, ED capacity, increased availability of virtual options).
Background
The National Committee for Quality Assurance (NCQA) developed Healthcare Effectiveness Data and Information Set (HEDIS) to provide purchasers and consumers with a comprehensive set of standardized performance measures to allow to assess health plan performance. Certain HEDIS measures specifically track follow-up care after an ED visit for mental health and alcohol or other substance use disorders (SUD) to quantify what proportion of behavioral health patients receive care within seven and 30 days.3,4 Beyond the 30-day period, HEDIS measures do not track whether patients received any additional care, whether in an ED or other care setting.
Analytic Approach
To understand behavioral health patient journeys following an ED visit, we identified patients who were treated in the ED for either anxiety, depression, alcohol or SUD. We focused our analysis on patients who were continuously enrolled in a health plan for 60 days following the ED visit to capture all healthcare encounters. Within that 60-day follow-up period, we first analyzed how many days lapsed between the ED visit and a follow-up visit with a behavioral health provider (inpatient treatment for alcohol and SUD) to understand if any follow-up care was delivered. Second, we identified the care settings that patients visited within a 30-day follow-up period, specifically for the same visit reason as the ED visit. Those care settings were limited to primary care, behavioral health, ED and inpatient treatment.
Findings
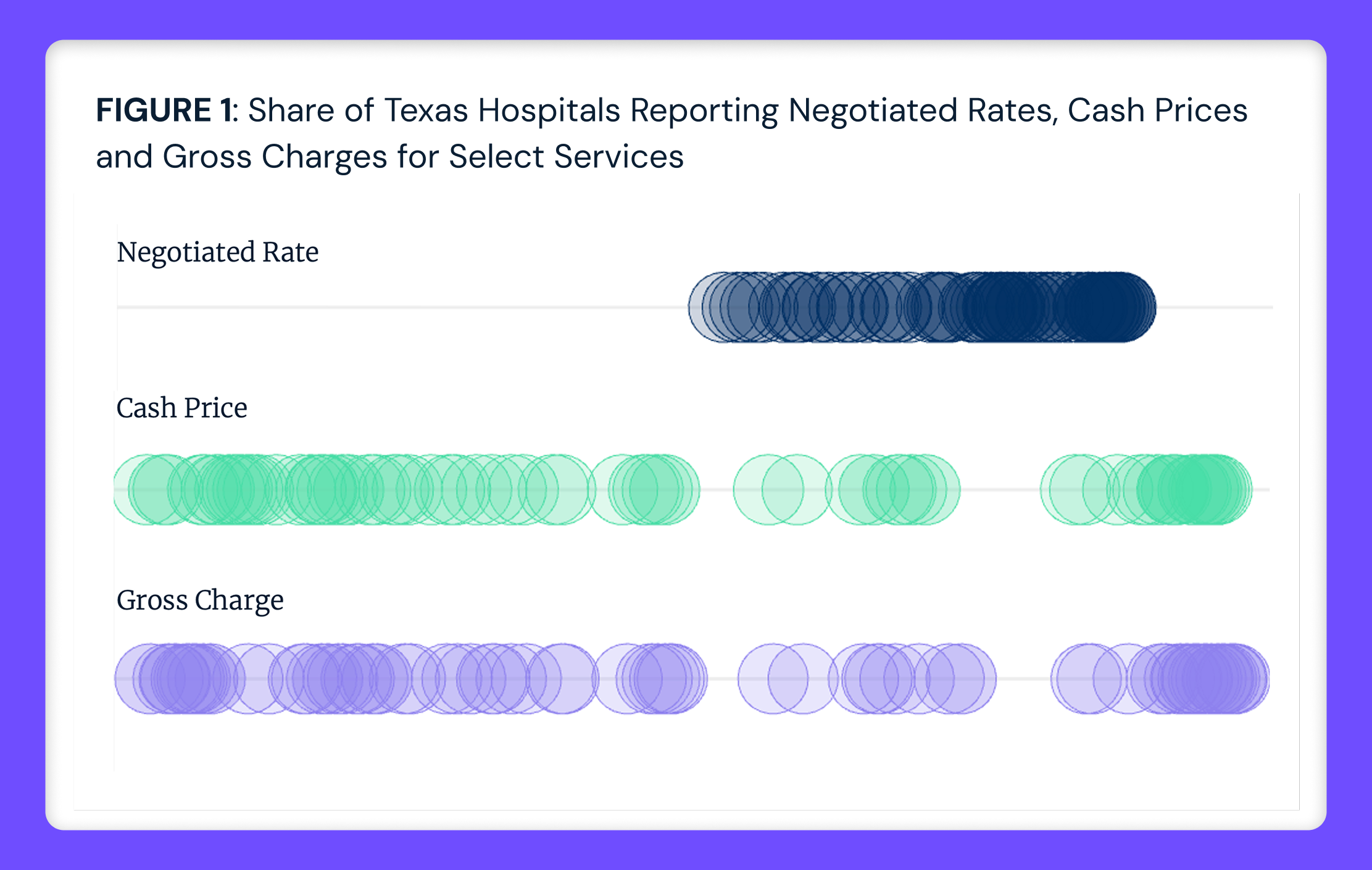
Most behavioral health patients, particularly those with alcohol or SUD, do not receive follow-up care after an ED visit. Half of patients who were treated in an ED for anxiety or depression did not receive care from a behavioral health provider within 60 days (Figure 1). Over 80% of patients who were treated in an ED for an alcohol or SUD did not receive inpatient care within 60 days.
Almost 10% of patients with alcohol or SUD are treated in an ED within 30 days, as compared to 5.9% of anxiety and depression patients within that timeframe. While 26.8% of patients who were treated in the ED for anxiety or depression received care from a behavioral health provider within 30 days, that share was only 10.0% for patients with alcohol or SUD.
While fewer patients are going to the ED for treatment of behavioral health conditions post-pandemic, it is evident that a substantial share of patients initially seeking treatment in the ED are not receiving specialized follow-up care. As ED capacity has progressively become less overwhelmed with COVID-19, and thus behavioral health volumes could return to or exceed pre-pandemic levels, how will these patients receive proper treatment given ongoing staffing constraints?
Without proper treatment of diagnosed behavioral health conditions, patients will face an increased risk of exacerbating the effects of other physical co-morbidities. Ultimately, if a scenario where an increasing share of behavioral health conditions goes untreated, total cost of care for those patients will continue to rise. We are currently in a position to mitigate rising costs across the healthcare system, so taking steps to shore up availability of provider supply to address the growing demand has never been more important. The specific ways in which behavioral health conditions can increase total cost of care will be explored in subsequent research.
- Specialty Care
- Behavioral Health






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)