Research
Leveraging Risk Adjustment to Analyze Health Status of Patients Receiving Cancer Treatment in 2017 and 2022
Mar 31, 2024 12:01:00 AMKey Takeaways
-
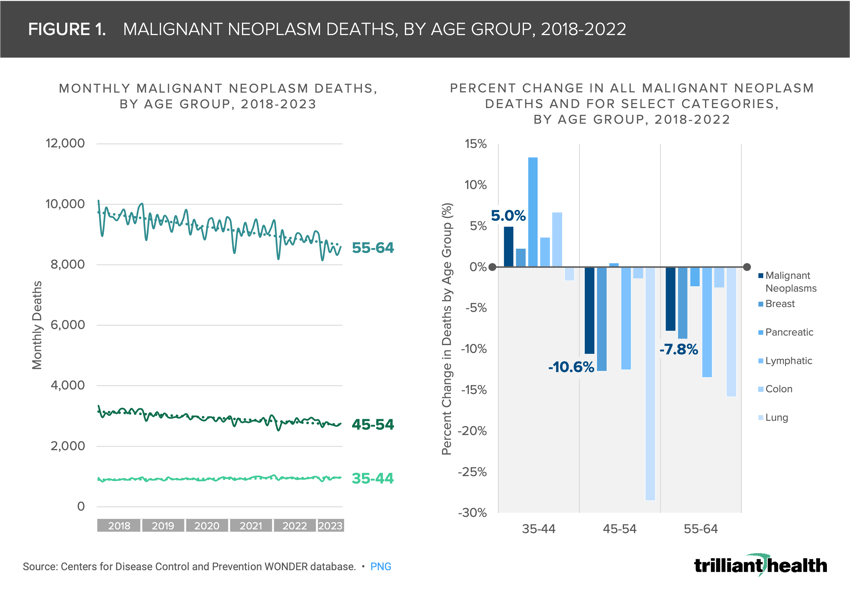
Missed screenings and delayed diagnoses have exacerbated advanced-stage presentations and increased mortality rates among cancer patients, particularly in younger age groups, where deaths from malignant neoplasms increased by 5.0% among individuals aged 35-44 from 2018 to 2022.
-
For certain cancers, patients being treated in 2022 were generally healthier than patients with the same diagnosis in 2017, notably for breast cancers and colon cancers. While this trend was not universal across all cancer types studied, with certain cancers showing negligible changes in health status, it will be an important dynamic to monitor closely.
In previous research, we studied the factors influencing cancer incidence, prevalence and mortality in the U.S. These trends present enduring and emerging disease management challenges.1
Many stakeholders believe that disruptions caused by the COVID-19 pandemic led to an increase in missed screenings and delayed diagnoses, creating concerns about advanced-stage presentations and mortality rates.
Given these findings, we were interested in examining the health status of patients receiving treatment for select cancers in 2017 compared to 2022.
Background
The number of new cancer cases in the U.S. increased steadily from 1999 through 2019, from 1.3M to 1.8M, highlighting the growing burden of cancer in aggregate. Although national cancer mortality rates have generally declined over time, there is meaningful variation by age group.2
Younger age groups historically are less affected by many cancers, which is reflected in current cancer screening guidelines. However, from 2018 to 2022, deaths from malignant neoplasms increased by 5.0% among individuals ages 35-44 (Figure 1). Conversely, malignant neoplasm deaths have decreased year-over-year for older age groups, specifically ages 45-54 and 55-64.
Increasing acuity in younger Americans without pre-existing conditions, in tandem with the projected cancer incidence and mortality rates, underscore concerns about worsening acuity and incidence since the COVID-19 pandemic. Media coverage highlighting the rise of colorectal cancer cases, especially among younger individuals, is increasingly prevalent.3,4,5 In 2024, the American Cancer Society estimates that there will be 2.0M new cancer cases and 611K cancer deaths in the U.S.6
Analytic Approach
Leveraging Trilliant Health’s national all-payer claims database and the Centers for Medicare and Medicaid Services (CMS) Hierarchical Condition Category (HCC) prospective risk adjustment methodology to calculate risk adjustment factor (RAF) scores, we compared the health status of patients receiving treatment for colon cancers, cervical cancers, breast cancers, lung cancers and select blood cancers in 2017 and 2022.7,8
HCCs are derived from ICD-10 diagnosis codes, focus on chronic health conditions and incorporate gender and age in the categorization. HCCs exclude non-diagnostic diagnoses (e.g., abdominal pain), clinically insignificant diagnoses (e.g., a sprain) or diagnoses that are definitively treated (e.g., acute appendicitis). Patients with RAF scores less than 1.0 are considered relatively healthy.
While the CMS-HCC model is used to estimate future expenditures for Medicare beneficiaries, our analysis used the model as an indication of health status for commercially insured patients. The analysis was limited to patients under age 65 with at least two visits associated with their cancer diagnosis in the given calendar year.
Findings
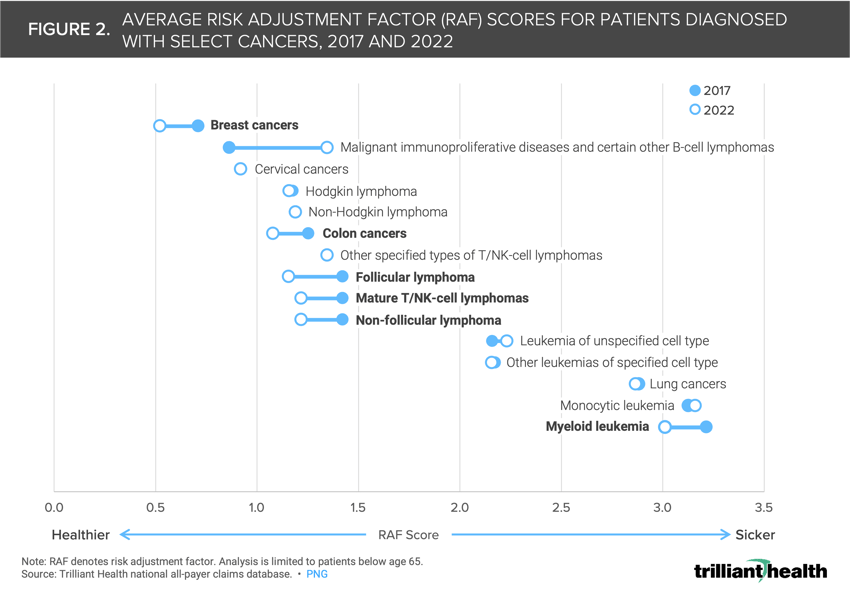
Comparing average RAF scores across different cancer types revealed shifts in health status between 2017 and 2022.
In 2022, breast cancers, colon cancers, follicular and non-follicular lymphoma, mature T/NK-cell lymphomas and myeloid leukemia exhibited lower average RAF scores compared to 2017 (Figure 2). For instance, the average RAF score for colon cancers decreased to 1.080 in 2022, a 13.9% decline from the 2017 average.
Conversely, cervical cancers, Hodgkin lymphoma, non-Hodgkin lymphoma, specified types of T/NK-cell lymphomas and monocytic leukemia showed negligible changes in average RAF scores.
However, malignant immunoproliferative diseases, certain B-cell lymphomas and leukemia of unspecified cell types displayed higher average RAF scores in 2022 compared to 2017.
Median Patient Age of Patients Receiving Cancer Treatment Over Time
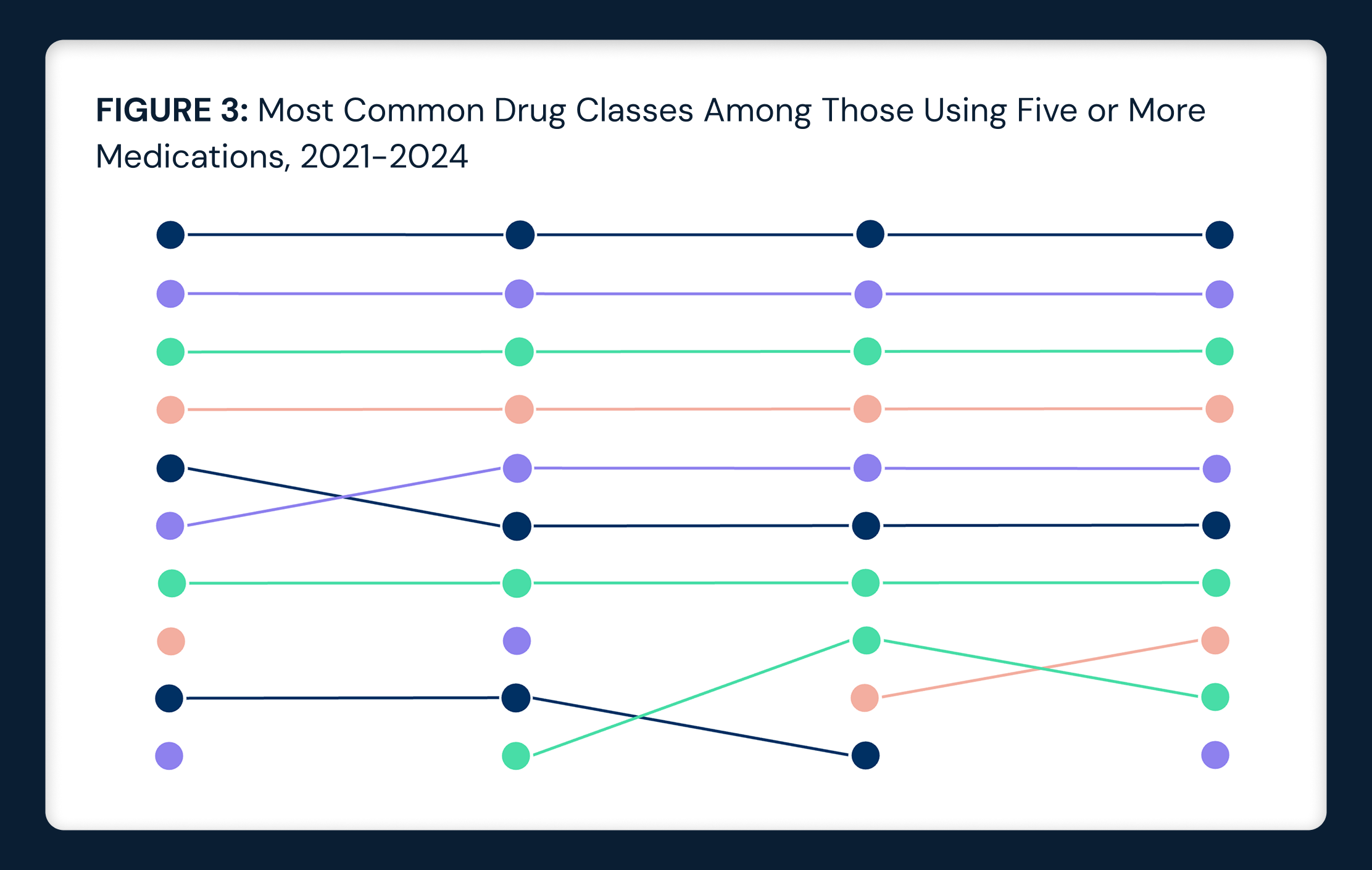
Analyzing the median age of patients receiving treatment for colon cancers, cervical cancers, breast cancers, lung cancers and select blood cancers in 2017 and 2022 reveals that the median age has slightly declined for some, but not all, cancers analyzed. The median patient ages for Hodgkin lymphoma, leukemia of unspecified cell types and mature and other specified types T/NK-cell lymphomas patients were slightly lower in 2022 than in 2017 (Figure 3). Specifically, the median age for leukemia of unspecified cell types decreased from 45 to 42. There was no change in median age for follicular and non-follicular lymphoma, malignant immunoproliferative diseases and certain other B-cell lymphomas, breast cancers, cervical cancers, colon cancers, myeloid leukemia, other specified and unspecified types of non-Hodgkin lymphoma. The median age increased by one year in 2022 compared to 2017 for lung cancers and other leukemias of specified cell types.

Conclusion
Utilizing risk adjustment reveals a signal that, for certain cancers, patients being treated in 2022 were generally healthier than patients with the same diagnosis in 2017, evidenced by lower average RAF scores, notably for breast cancers and colon cancers. While this trend was not universal across all cancer types studied, with certain cancers showing negligible changes in health status, it will be an important dynamic to monitor closely.
These findings raise several issues of concern. What might explain an increase in diagnoses of certain – but not all – cancers in populations that are healthier based upon RAF scores? Are there clinical similarities among the cancer types that increased? When did these changes first appear? Are there clinical differences between the cancer types that increased and those that showed little change?
The increase in cancer diagnoses in relatively healthier patients, the increasing mortality in younger cancer patients and the projections of further increases in cancer prevalence underscore the urgent need for proactive measures. These measures may include, but should not be limited to, adjusting cancer screening guidelines.
Thanks to Matt Fili, Colin Macon, Alli Oakes and Katie Patton for their research support.
- Specialty Care
- Disease Burden






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)