Key Takeaways
-
Inconsistent commercial coverage of both bariatric surgical procedures and specific drugs like semaglutide will further fragment access to weight loss procedures and treatments.
-
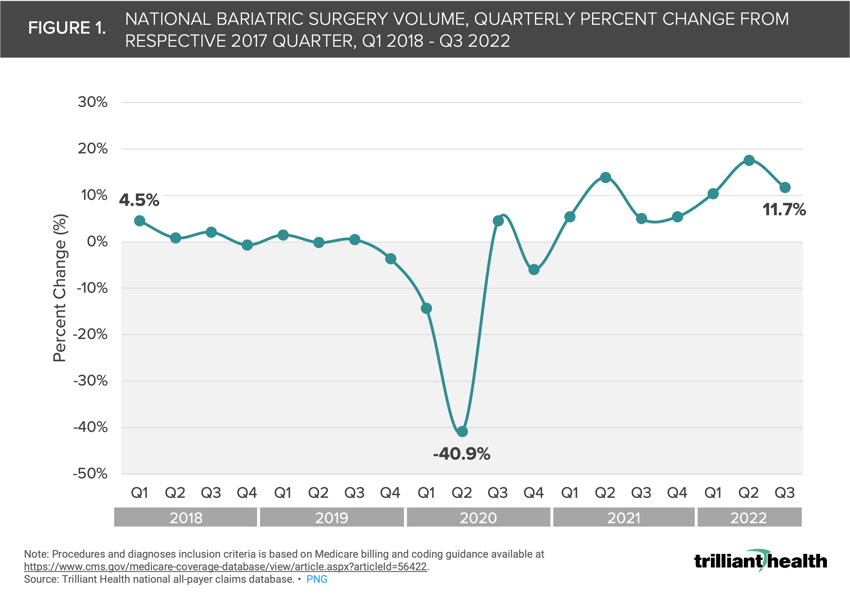
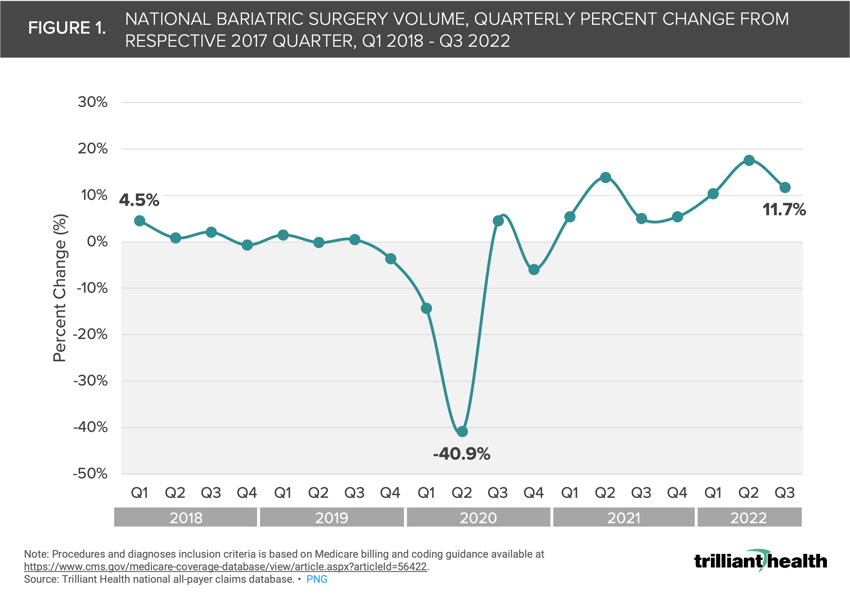
While bariatric surgery procedure volume dropped at the onset of the COVID-19 pandemic, volumes began to rebound in Q1 2021. In 2018 and 2019, quarterly comparisons to 2017 ranged from -3.7% (Q4 2019) to +4.5% (Q1 2019).
-
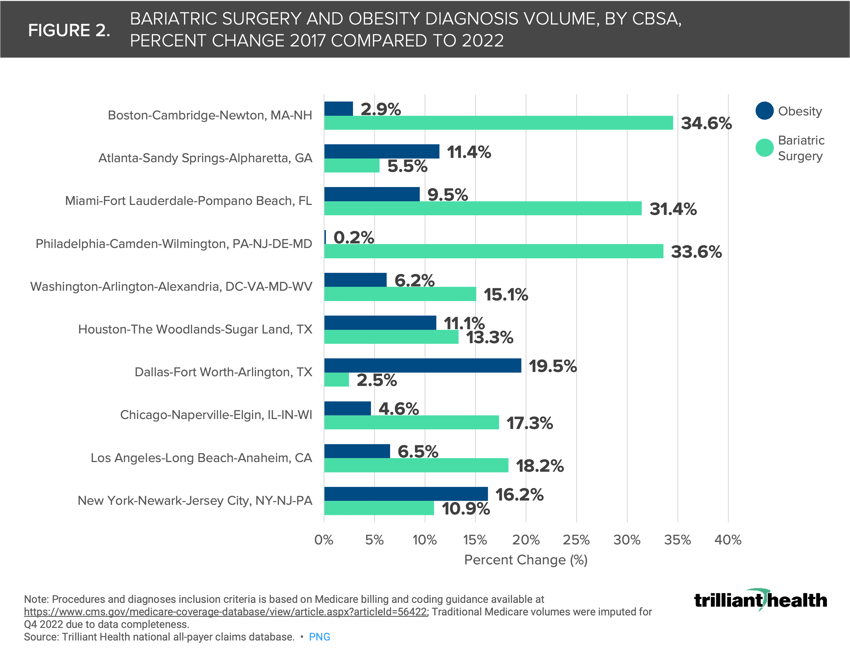
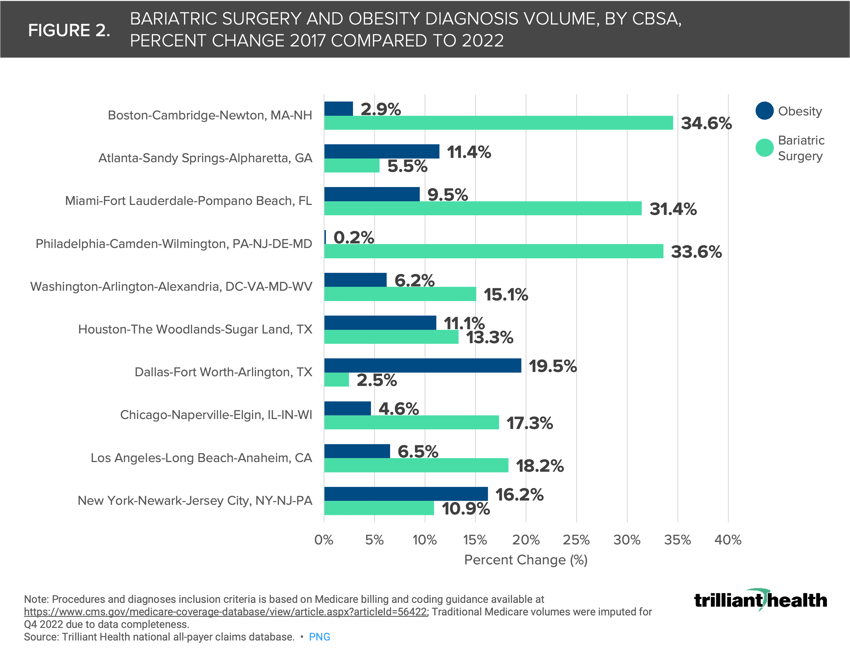
Although national bariatric surgical procedure volumes began to rebound in 2021, regional volume changes for bariatric surgery have not aligned with changing obesity prevalence. For example, bariatric surgical procedures (+33.6%) are far outpacing obesity diagnoses (+0.2%) in Philadelphia, PA.
The demand for prescription drug use for the treatment and management of Type 2 diabetes and obesity—specifically semaglutide—is unprecedented. Previously, bariatric surgery was the primary treatment for obesity, but it was invasive, costly—albeit a one-time cost compared to a lifetime of monthly semaglutide injections—and lacked consistent commercial insurance coverage.1 With increased demand for semaglutide, growing obesity prevalence and rising healthcare expenditures, we were curious to explore how demand for bariatric surgical procedures has changed in tandem.
Background
By Q3 2022, patient volumes for semaglutide weight loss drugs increased 355% from Q1 2020, with the largest share of patients (35.9%) being females ages 45 to 64.2 The combination of unprecedented demand for these drugs and America’s obesity crisis (41.9% of American adults) suggests that semaglutide will provide an alternative to bariatric surgery.3 However, the longer-term impacts on bariatric surgical demand will take years to fully understand, as these drugs entered the market between 2017 and 2022.
Earlier this year, the American Academy of Pediatrics revised guidelines to include weight loss drugs like semaglutide and bariatric surgery for the evaluation and treatment of children ages 12 and older with diagnosed obesity.4 Bariatric surgery is now recommended for pediatric patients ages 12 and over with a body mass index (BMI) greater than 35, but weight loss drugs have broader criteria for pediatric obesity management. Although these guidelines have changed, it remains to be seen whether parents adopt these practices and whether drug supply will meet demand for a younger patient cohort.5 A recent study utilizing registry data through 2021 found volume increases in certain types of bariatric surgery for both adults and children.6
Although demand for weight loss interventions is expected to persist across all age groups, cost is a significant barrier to access. Weight loss surgery can cost between $7,400 to $33,000 before insurance, while semaglutide costs can range from $892 to $1,300+ per month.7,8 Inconsistent commercial coverage for both bariatric surgical procedures and drugs like semaglutide further fragment access to weight loss procedures and treatments.9 In contrast, Medicare and Medicaid offer more consistent coverage, provided certain medical necessity criteria are met, such as a BMI above 35 and evidence of failed diet and exercise programs.10
Analytic Approach
We studied the magnitude change in bariatric surgery nationally and regionally relative to the change in obesity disease burden. Using national all-payer claims data, we examined volume of bariatric surgical procedures and obesity diagnoses between Q1 2017 and Q3 2022. Inclusion criteria for bariatric surgical procedures was determined using Medicare billing and coding guidance.11 Regional trends in bariatric surgery and obesity diagnoses were also analyzed, focusing on the 10 largest CBSAs by population size.
Discussion
While the volume of bariatric surgery procedures initially dropped during the COVID-19 pandemic, it began to rebound in Q1 2021. Quarterly comparisons to 2017 ranged from -3.7% to +4.5% in 2018 and 2019 (Figure 1). The peak quarterly growth of +17.4% occurred in Q2 2022, but the aggregate volumes remained relatively stable before and after Q2 2020. This rebound can be attributed to hospitals resuming all elective procedures following the COVID-related pauses.
In Houston, TX, the percent change in obesity diagnoses (+11.1%) and bariatric surgery procedures (+13.3%) between 2017 and 2022 were relatively similar. However, in Philadelphia, PA, bariatric surgical procedures (+33.6%) significantly outpaced obesity diagnoses (+0.2%) as shown in Figure 2.
Compass+ Exclusive: Segmenting Bariatric Surgery Trends by Age

Although national bariatric surgical procedure volumes began to recover in 2021, regional changes in volume did not align with changes in obesity prevalence. The widespread use of semaglutide, both on- and off-label use, and the pediatric guideline changes for addressing obesity underscore the nation’s prioritization of curbing the prevalence of obesity. Whether clinicians and guardians will introduce surgical and medication intervention more commonly during childhood remains to be seen.
Similarly, whether medication management for weight loss will overtake bariatric surgery as the “gold standard” is an open question. The long-term side effects of these therapies, which are designed for lifelong use, and their cost implications, which can exceed $1,000 per month, are still being studied. With healthcare spending approaching 20% of U.S. GDP, the increasing demand for expensive weight loss drugs and weight loss surgical procedures will profoundly impact national healthcare expenditures.
Tracking the impact of weight loss drugs on bariatric surgery over time is crucial. To what extent are the patients taking semaglutide for off-label use widening the gap for patients with greater clinical need? What side effects may manifest from off-label use? Will drugs like semaglutide serve as a substitute or alternatives to bariatric surgery? Will the patient demographics of bariatric surgery patients be similar or vastly different to those using long-term weight loss medications? Monitoring these trends will be critical in understanding obesity disease burden and the associated costs to the U.S. healthcare system.






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)