Research
Growth in Emerging Chronic Conditions Signals a General Sense of Unwellness
November 3, 2025Study Takeaways
- Between 2021 and 2024, prevalence increased most sharply for long COVID (68.0%), obstructive sleep apnea (46.3%) and NAFLD/NASH (27.0%), reflecting growing recognition of metabolic, respiratory and post-viral disease burden.
- POTS (43.3%), endometriosis (19.4%) and thyroid dysfunction (20.9%) saw the largest relative increases among women, while male patients saw the greatest increases in sleep apnea (41.0%) and NAFLD/NASH (22.2%).
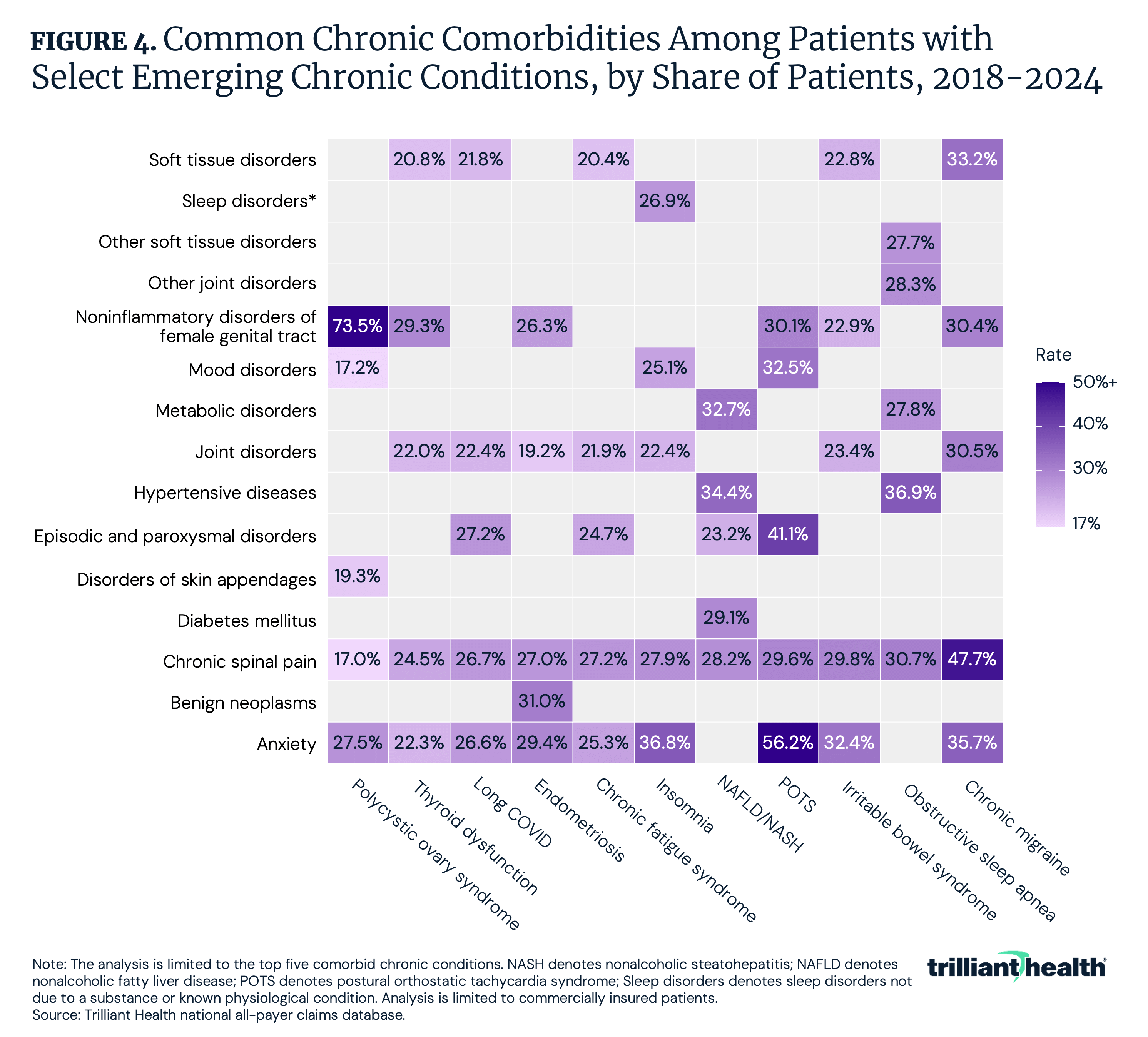
- Chronic spinal pain, anxiety and soft tissue and joint disorders were the most common comorbidities among patients with select emerging chronic conditions.
A subset of emerging chronic conditions has received increased clinical attention in recent years. Conditions such as postural orthostatic tachycardia syndrome (POTS), long COVID, nonalcoholic fatty liver disease (NAFLD)/nonalcoholic steatohepatitis (NASH) and polycystic ovary syndrome (PCOS), previously characterized by limited research investment and inconsistent diagnostic criteria, have appeared more commonly in medical literature, media coverage, social media and patient advocacy discourse. This study examines the diagnostic patterns for these conditions, segmenting by patient demographics and analyzing common comorbidities. The conditions examined in this study represent a heterogeneous group spanning multiple clinical domains and body systems. They range from well-established diagnoses with standardized treatment protocols (e.g., obstructive sleep apnea) to conditions that have only recently received formal recognition (e.g., POTS) or even remain incompletely understood (e.g., chronic fatigue syndrome).
Background
Chronic conditions are a leading cause of disability, lost productivity and out-of-pocket healthcare spending. As of 2023, 76.4% of adults had least one chronic condition, and more than half have at least two chronic conditions.1 Reflecting the magnitude of this issue, approximately 90% of U.S. healthcare expenditures are attributed to individuals with chronic and mental health conditions.2
Conditions such as NAFLD/NASH and obstructive sleep apnea have been diagnosed at a growing rate over the past two decades, driven by expanded diagnostic criteria and growing recognition of their association with metabolic and cardiovascular diseases, such as hypertension and obesity. However, underdiagnosis is still prominent.3,4 Time to diagnosis also poses another problem for these patient populations. Endometriosis, for example, typically requires 7-10 years from symptom onset to diagnosis, and PCOS affects an estimated 6-13% of women of reproductive age, yet remains underdiagnosed at a rate of 70%.5,6 The underdiagnosis and delayed diagnosing underscore both the complexity of differential diagnosis and lack of sufficient research on conditions predominantly affecting women.
Other conditions examined in this study have gained prominence through different pathways. POTS and chronic fatigue syndrome have historically been difficult to conclusively diagnose, as they are conditions characterized by multi-system symptoms and limited objective biomarkers. POTS was also not recognized as a distinct diagnosis in ICD-10-CM coding until 2023. Recent years have seen increased clinical attention to these conditions, partly attributable to the emergence of long COVID, which has overlapping symptoms with several post-viral syndromes.7,8 Long COVID was also not recognized in the ICD-10-CM coding until 2021. The formal recognition of these conditions with a distinct diagnosis in ICD-10-CM coding can provide examples of how diagnosing behavior can shift when coding infrastructure is in place.
From a health economics perspective, these emerging chronic conditions have implications for healthcare spending. In 2016, direct healthcare costs for treating chronic conditions were estimated at $1.1T.9 Many of these conditions lack curative therapies and receive ongoing symptom management, specialist consultation, diagnostic testing and high-cost pharmaceutical intervention. The economic burden of managing conditions such as endometriosis ($78-119B) and NAFLD/NASH ($222.6B) can be substantial.10,11
Perhaps unsurprisingly, research has documented that direct-to-consumer advertising, health information websites and social media platforms can influence patient care-seeking behavior and diagnostic requests.12,13 The extent to which increased visibility of certain conditions through news and social media platforms influences disease “prevalence” is an important research area.
By examining several emerging chronic conditions, this analysis provides context for condition-specific demographic patterns and common comorbidities.
Analytic Approach
Leveraging national all-payer claims, commercial visits associated with diagnoses for the following conditions were examined between 2018 and 2024:
- Chronic fatigue syndrome
- Chronic migraine
- Endometriosis
- Insomnia
- Irritable bowel syndrome (IBS)
- Long COVID
- NAFLD/NASH
- Obstructive sleep apnea
- PCOS
- POTS
- Thyroid dysfunction (e.g., hypothyroidism, Hashimoto’s)
Non-elderly adult patients diagnosed with these conditions were segmented by gender and age group: 18-44 and 45-64. The most common chronic comorbid conditions associated with each condition were also analyzed.
Findings
Between 2021 and 2024, most emerging chronic conditions increased in prevalence, with the largest relative growth observed in long COVID (68.0%), obstructive sleep apnea (46.3%) and NAFLD/NASH (27.0%) (Figure 1). In 2023, a formal ICD-10 diagnosis was established for POTS, which resulted in a 34.0% increase from 2023 to 2024.
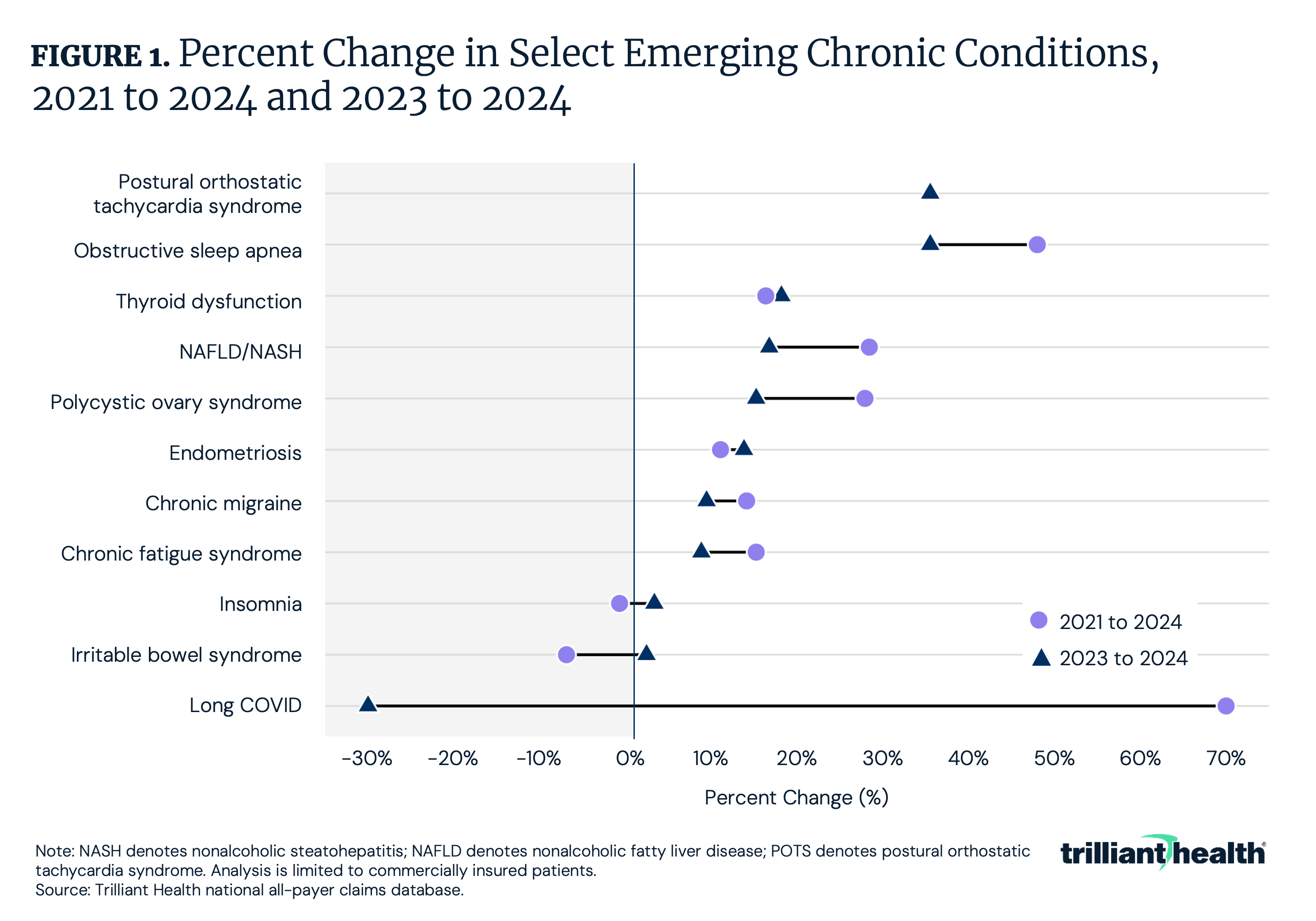
Between 2023 and 2024, patient volume for emerging chronic conditions showed relatively consistent growth across genders, with modest variation in magnitude by condition. Among females, the largest relative increases were observed in POTS (43.3%), endometriosis (19.4%) and thyroid dysfunction (20.9%) (Figure 2). Among males, growth was most pronounced for obstructive sleep apnea (41.0%), POTS (34.1%) and NAFLD/NASH (22.2%). Long COVID declined equally across both groups (-26.0%).
 Between 2023 and 2024, the change in patient volume varied between nonelderly adult age groups among select emerging chronic conditions. Among adults ages 18-44, the largest relative increases were observed in POTS (45.6%), obstructive sleep apnea (39.9%) and NAFLD/NASH (22.2%). For adults ages 45-64, the largest increases were in obstructive sleep apnea (61.6%) and NAFLD/NASH (26.9%) (Figure 3). Long COVID declined among adults 18-44 (-25.2%) and 45-64 (-55.5%).
Between 2023 and 2024, the change in patient volume varied between nonelderly adult age groups among select emerging chronic conditions. Among adults ages 18-44, the largest relative increases were observed in POTS (45.6%), obstructive sleep apnea (39.9%) and NAFLD/NASH (22.2%). For adults ages 45-64, the largest increases were in obstructive sleep apnea (61.6%) and NAFLD/NASH (26.9%) (Figure 3). Long COVID declined among adults 18-44 (-25.2%) and 45-64 (-55.5%). Across emerging chronic conditions, there is a relatively high comorbidity prevalence of chronic pain, anxiety and metabolic disorders. Chronic spinal pain (e.g., back and neck pain) is the most common comorbid diagnosis across nearly all conditions, ranging from 24.5% of patients with thyroid dysfunction to 47.7% of those with chronic migraine (Figure 4). Similarly, joint and soft tissue disorders are common among this patient population. Anxiety and stress-related disorders are also highly prevalent, appearing among 36.8% of patients with insomnia, 32.4% with IBS, 29.4% with endometriosis, 25.3% with chronic fatigue syndrome, 35.7% with chronic migraine and 56.2% among those with POTS. Female-specific comorbidities such as noninflammatory disorders of the female genital tract feature prominently among conditions with high female prevalence, including 73.5% of PCOS patients, 30.4% of chronic migraine patients and 26.3% of endometriosis patients. Metabolic and cardiovascular conditions (i.e., hypertension, metabolic disorders and diabetes) dominate among NAFLD/NASH and obstructive sleep apnea, affecting between 27% and 37% of patients.
Across emerging chronic conditions, there is a relatively high comorbidity prevalence of chronic pain, anxiety and metabolic disorders. Chronic spinal pain (e.g., back and neck pain) is the most common comorbid diagnosis across nearly all conditions, ranging from 24.5% of patients with thyroid dysfunction to 47.7% of those with chronic migraine (Figure 4). Similarly, joint and soft tissue disorders are common among this patient population. Anxiety and stress-related disorders are also highly prevalent, appearing among 36.8% of patients with insomnia, 32.4% with IBS, 29.4% with endometriosis, 25.3% with chronic fatigue syndrome, 35.7% with chronic migraine and 56.2% among those with POTS. Female-specific comorbidities such as noninflammatory disorders of the female genital tract feature prominently among conditions with high female prevalence, including 73.5% of PCOS patients, 30.4% of chronic migraine patients and 26.3% of endometriosis patients. Metabolic and cardiovascular conditions (i.e., hypertension, metabolic disorders and diabetes) dominate among NAFLD/NASH and obstructive sleep apnea, affecting between 27% and 37% of patients.
Conclusion
Few, if any, health economy stakeholders would dispute that chronic and co-morbid conditions are a key contributor to America’s healthcare cost crisis. As a result, any increase in the number or prevalence of chronic conditions is problematic.
The recent increase in certain metabolic, respiratory and post-viral conditions, coupled with numerous chronic comorbidities, confirms that the American public is increasingly unwell. The most important and concerning proof point is that the crude mortality rate among adults ages 18-44 increased from 349.8 in 2018 to 366.7 per 100,000 in 2023.
These findings present different challenges for different healthcare stakeholders. A key consideration for Federal and state policymakers is how to balance support for healthcare needs with encouragement of healthy lifestyle choices. While many chronic conditions have genetic components, research shows that lifestyle factors play a significant role in preventing or managing many chronic health conditions.
For health systems and medical groups, understanding demographic and utilization patterns enables more accurate demand forecasting and capacity planning. The high comorbidity burden suggests potential value in integrated care models that address multiple related conditions rather than managing each diagnosis independently.
For life sciences companies, therapeutic interventions are increasingly used instead of or in combination with procedural interventions for patients who are more medically complex. However, therapeutic advances that delay or prevent procedural interventions can create tension between clinical optimization and the economic reality that procedures represent a substantial portion of healthcare revenue.
For payers, the demographic concentration of certain conditions and associated comorbidity profiles inform actuarial modeling and benefit design decisions. More importantly, these trends call into question how medical loss ratio (MLR) dollars are being spent (i.e., the split between investments in health versus reimbursing providers for treating or managing illness). At a minimum, these data support consideration of condition-specific interventions focused on high-prevalence demographic segments, though cost-effectiveness analysis would be required to determine optimal intervention strategies.
Collectively, the challenge for health economy stakeholders is to consider its poor performance in managing predictable chronic health conditions. Policymakers have a responsibility to engage in open dialogue with their communities about the relationship between lifestyle factors and health outcomes, both for individuals and at the population level – and ultimately for the nation’s fiscal health. Other stakeholders, like providers and payers, have an obligation to amplify those messages and encourage and facilitate healthy lifestyle behaviors. Likewise, providers and life sciences companies have an obligation to collaborate to provide the most clinically efficacious and cost-effective treatment for common chronic conditions based on long-established frameworks like quality-adjusted life years. The health of Americans, and America, is what is at stake.
- Studies






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)