Trilliant Health
Use Cases

Develop Service Line Strategies

Analyze the Competitive Landscape

Anticipate Future Patient Needs

Identify Sites To Capture Demand

Drive Loyalty Across the Patient Journey

Leverage Price Transparency Insights

Retain Patients in Your Network

Match Provider Supply to Demand
Industries

Acquire Commercial Patients

Capture Outpatient Demand

Target High-Value HCPs

Strengthen Provider Networks
Our Data
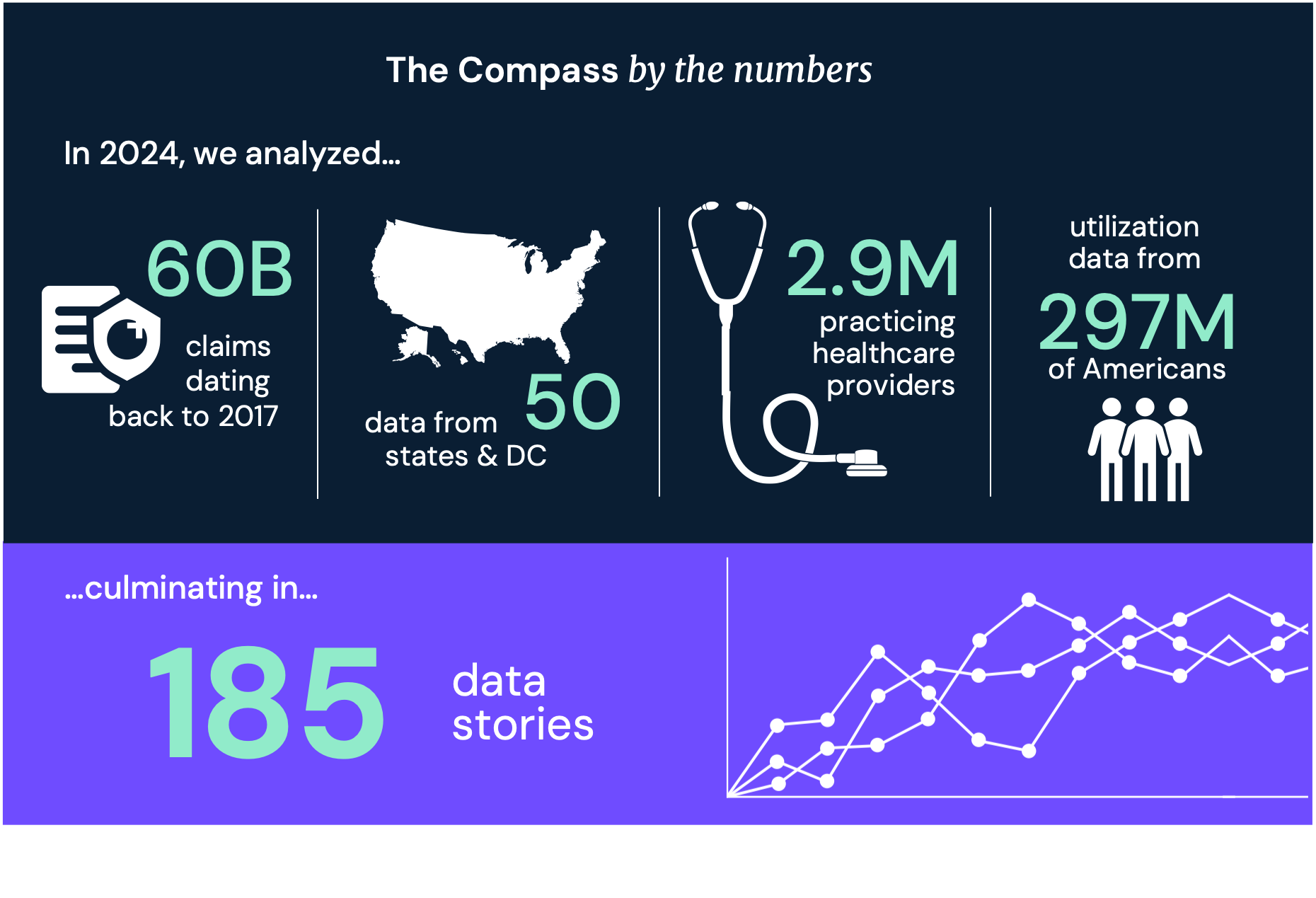
We collect and organize the industry’s most comprehensive healthcare datasets.
Data Pipelines
See demand, supply and yield across the U.S. health economy

Validated Data for 2.9M Practitioners

Episodes of Care for 300M Patients

Negotiated Rates for Any Service at Any Location
Ways to Access
Resources
Flexible solutions to fit your specific needs and workflow
Free resources to help health economy stakeholders use our products and data

Answer Key Questions in Seconds
AI Chatbot for Hospital Prices

Custom Enterprise-Level Analyses

Data-Driven Benchmarking Tool

Inform Data-Driven Strategies

Health Economy Survival Strategies

Product Guides and Feature Releases

Strategic guidance and commentary from our CEO, Hal Andrews
.png)
Analysis of trends shaping the health economy

Original research on trends shaping the health economy
Use Cases

Develop Service Line Strategies

Analyze the Competitive Landscape

Anticipate Future Patient Needs

Identify Sites To Capture Demand

Drive Loyalty Across the Patient Journey

Leverage Price Transparency Insights

Retain Patients in Your Network

Match Provider Supply to Demand
Industries

Acquire Commercial Patients

Capture Outpatient Demand

Target High-Value HCPs

Strengthen Provider Networks
Our Data
We collect and organize the industry’s most comprehensive healthcare datasets.
Data Pipelines
See demand, supply and yield across the U.S. health economy

Validated Data for 2.9M Practitioners

Episodes of Care for 300M Patients

Negotiated Rates for Any Service at Any Location
Ways to Access
Flexible solutions to fit your specific needs and workflow
Answer Key Questions in Seconds
Custom Enterprise-Level Analyses
Inform Data-Driven Strategies
Resources
Free resources to help health economy stakeholders use our products and data
AI Chatbot for Hospital Prices
Data-Driven Benchmarking Tool
Health Economy Survival Strategies
Product Guides and Feature Releases

Strategic guidance and commentary from our CEO, Hal Andrews
.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)
Analysis of trends shaping the health economy

Original research on trends shaping the health economy