The Compass
Sanjula Jain, Ph.D. | February 5, 2023Anxiety, Depression, Chronic Pain Among Common Diagnoses Preceding Endometriosis and PCOS Diagnosis
Key Takeaways
-
Research reveals considerable delays in accurately diagnosing individuals with endometriosis and polycystic ovary syndrome (PCOS), in turn delaying timely intervention to treat associated risks such as infertility.
-
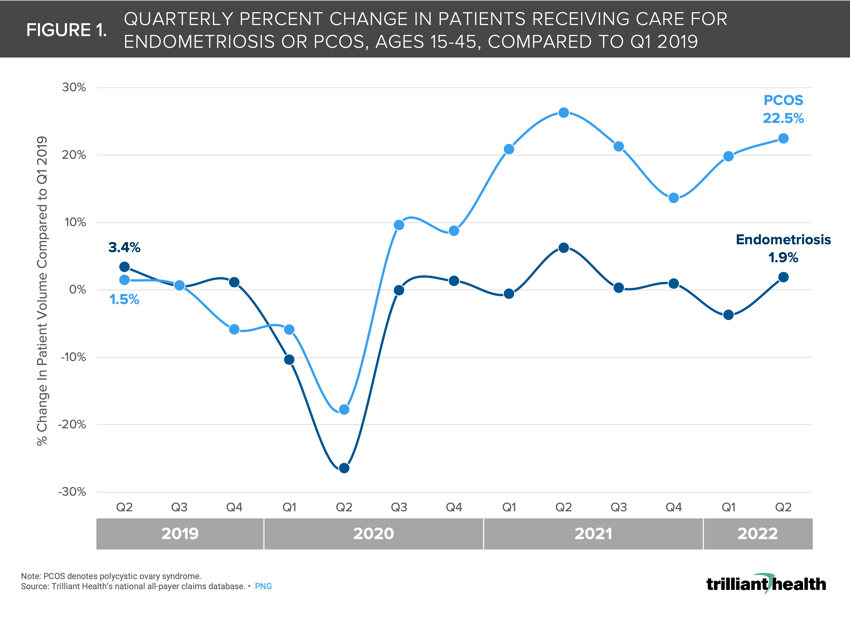
Overall, the volume of patients being treated for or diagnosed with endometriosis remained relatively stable (+1.9%) between Q1 2019 and Q2 2022 but increased for PCOS by +22.5% over the same period.
-
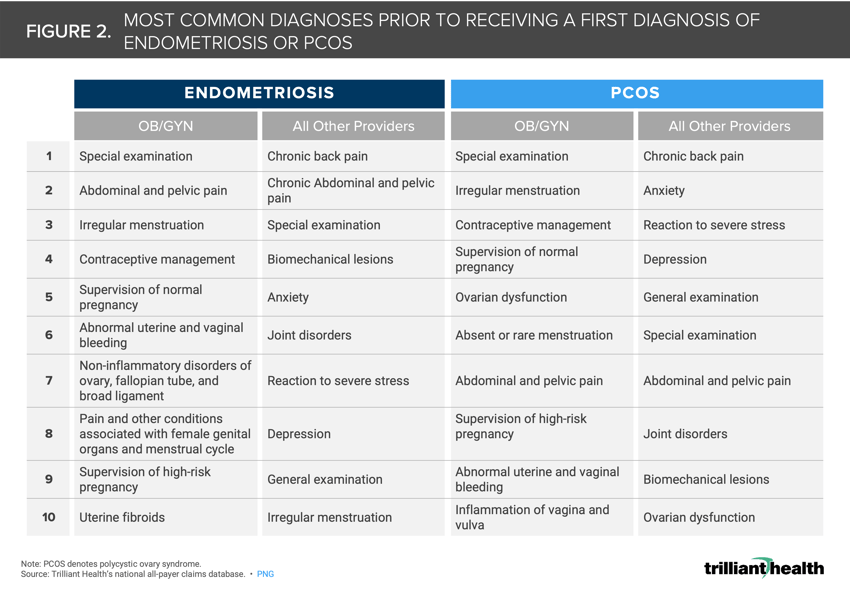
Non-specific diagnoses including irregular menstruation, abdominal pain and abnormal bleeding rendered by OB/GYNs were common among both PCOS and endometriosis patients prior to receiving a formal diagnosis.
Investments in women’s healthcare services are expected to increase again this year, particularly for fertility services. Even so, the industry lacks timely research that quantifies the national landscape and magnitude of women’s health conditions.1,2 Two conditions in particular, endometriosis and PCOS, are worthy of further study to support improvements in accurate and timely diagnosis and treatment.
Background
Endometriosis is a condition characterized by endometrial tissue growing outside of the uterus, with common symptoms including chronic pain, bleeding, and digestive issues. While endometriosis affects roughly 10% of women of reproductive age, commonly cited research studying incidence is more than a decade old and focused on a small patient cohort.3,4,5
PCOS is the most common endocrine disorder of reproductive-aged women globally, with cited prevalence ranging from 6% to 10%.6,7,8 While the exact cause is unknown, PCOS stems from imbalanced reproductive hormones and can cause irregular menstruation, infertility, ovarian cysts, insulin resistance and other physical symptoms (e.g., weight gain, acne).
Research has determined there are considerable delays in accurately diagnosing endometriosis and PCOS, in turn delaying timely interventions to treat associated conditions like infertility.9,10,11
Analytic Approach
To understand more recent diagnostic patterns and trends for these two conditions, we identified patients in our national all-payer claims database with a first recorded diagnosis of either PCOS or endometriosis between 2019 and 2022. Our analysis was limited to women between the ages of 15 and 45 enrolled in either Medicaid or commercial insurance. To determine a patient’s first diagnosis, we required continuous enrollment between 2017 and 2022.
Findings
Overall, the volume of women being treated for or diagnosed with endometriosis remained relatively stable—despite a drop in early 2020 resulting from the COVID-19 pandemic—between 2019 and 2022, with just 1.9% more patients receiving care for endometriosis in Q2 2022 compared to Q1 2019 (Figure 1). However, the volume of women being treated for or diagnosed with PCOS has increased substantially since 2019—despite a drop in early 2020 resulting from the COVID-19 pandemic—with 22.5% more patients receiving care for PCOS in Q2 2022 compared to Q1 2019. Prior research has found that preventive primary care volumes for females ages 20-49 are higher as compared to pre-pandemic utilization, which may have contributed to the observed increase in PCOS detection.12
We next identified the most common diagnoses resulting from medical visits with OB/GYNs and all other provider types prior to a first diagnosis of either endometriosis or PCOS. For both conditions, the most common precursor conditions were similar. Care rendered for these common conditions by OB/GYNs were primarily non-specific diagnoses including irregular menstruation, abdominal pain, and abnormal bleeding (Figure 2). For non-OB/GYN providers, diagnoses such as chronic pain, reactions to severe stress, anxiety, and depression were most common prior to formal PCOS or endometriosis diagnosis. Findings from a genetic association study also found eating disorders, depression, and anxiety to be associated with endometriosis even after accounting for several comorbid conditions, including chronic pain.13
Standard delays from symptom onset to surgical diagnosis of endometriosis range from four to 11 years.14 Compared to pre-pandemic volumes, demand for behavioral health services has increased most for females (+26.2%).15 In 2020, 43 states reported their lowest general fertility rates in the last three decades, with 10 states experiencing reductions exceeding 20% over the last decade.16 These trends will be important to monitor going forward. Is the simultaneous increase in mental health disorders correlated with the sudden increase in PCOS diagnoses over the past three years, and, if so, will it continue? Will new investments in women’s health be able to reduce the time to diagnosis? Will this have a meaningful impact on recent infertility trends, or is there another factor at play? To what extent will the clinical pathways of treating OB/GYNs and other providers account for related diagnoses?
Given the considerably high prevalence of these conditions in women of reproductive age, investment focus on women’s health, and their known impact on fertility and chronic pain, more research for not only PCOS and endometriosis but on women’s health conditions writ large has never been more imperative.
Thanks to Kelly Boyce and Katie Patton for their research support.
- Women's Health
- Behavioral Health
- Disease Burden
You are currently viewing a free preview of our premium studies. To receive new studies weekly, upgrade to Compass+.
Sign UpSee more with Compass+
You are currently viewing the free version of this study. To access the full study and more leading research on the health economy, subscribe to Compass+.
Sign Up for Compass+