Counterpoint
Hal Andrews | February 2, 2021Winning a Losing Game, Part IV: Thinking About Customers – and Pricing – Like Amazon
“unlike health systems, consumer-focused enterprises do everything they can to understand consumers in their market, both customers and prospects, how much business the competition has, how and where to reach the customers of the competition, whether those customers are valuable, and how to take those customers away from the competition.”
One thing that every other industry outside of healthcare does is to understand customer preferences and price sensitivity for a basket of products. In their 2001 paper “Conditioning Prices on Purchase History”, Alessandro Acquisti and Hal R. Varian noted this:
“Many industries, including supermarkets, airlines, and credit cards, have compiled vast databases of individual consumer transactions and have used them to study purchase behavior and to make specific offers to individual consumers, via direct mail or other forms of targeted marketing. Many companies have become expert in using tracking tools to refine marketing strategies (see Bailey [1998], and Dayal et al. [2001]). Since so many transactions are now computer mediated, and these computers can easily be networked to data centers, sellers now have the ability to access databases of past purchases in real time. This allows them to condition current offers to consumers on their previous purchase behavior. Sellers can offer each individual a different price, a particular prize or coupon, or personalized recommendations. With computer mediated transactions, price discrimination on an individual basis becomes quite feasible.” [1]
As Barry C. Lynn noted last year in “The Big Tech Extortion Racket” in Harper’s Magazine,
“But Amazon’s license to discriminate is fast moving into something else, a system where each consumer is charged the maximum amount that he or she can pay. Many businesses have long dreamed of charging individual buyers different prices or delivering different levels of service for the same price. But until the advent of the internet and the ability to spy on the most intimate thoughts and actions of individuals, businesses could not do so effectively.” [2]
At first blush, this concept sounds nefarious. Upon reflection, this concept is simply a sophisticated algorithmic approach to something that health systems have done for decades: chargemaster management. The difference is that Amazon has a very specific strategy to maximize its yield from its customers, while health systems have a nebulous hope that a union official with a BCBS indemnity plan will walk through the door tomorrow.
Unlike Amazon, a hospital’s pricing strategy is completely divorced from the price that a consumer might willingly pay. This fact is a relic of how the healthcare system works, which a well-known health system executive describes this way: “exactly as it is designed.” Historically, health systems have rightly focused on the physician as the hospital’s customer for two reasons.
First, health systems are separated from their customer, always by the physician and often by health insurers and employers.
Second, consumers have never really objected to being treated as “patients” by hospitals and physicians. In fact, for decades “patients” have faithfully followed doctors’ orders, particularly with respect to referrals for services. As a result, healthcare providers have not been required to market or sell their services to the end users of those services to increase market share.
That approach is no longer sufficient. Irrespective of healthcare policy, healthcare economics continue to incentivize the migration of healthcare services delivery from inpatient to outpatient settings. This trend will accelerate as the Centers for Medicare and Medicaid Services (CMS) increases the number and type of procedures that can be performed in outpatient settings and eliminates the “inpatient only” list by 2024. [3] And, as a result of the pandemic, healthcare consumers have (finally) realized that healthcare services can be accessed in a variety of ways.
Will consultants continue to recommend that chargemasters be set at 400-500% of Medicare rates? Yes. Will that help your system influence consumers to make decisions in your favor? No, because consumers are increasingly sensitive to their increasing out-of-pocket costs, as shown here:
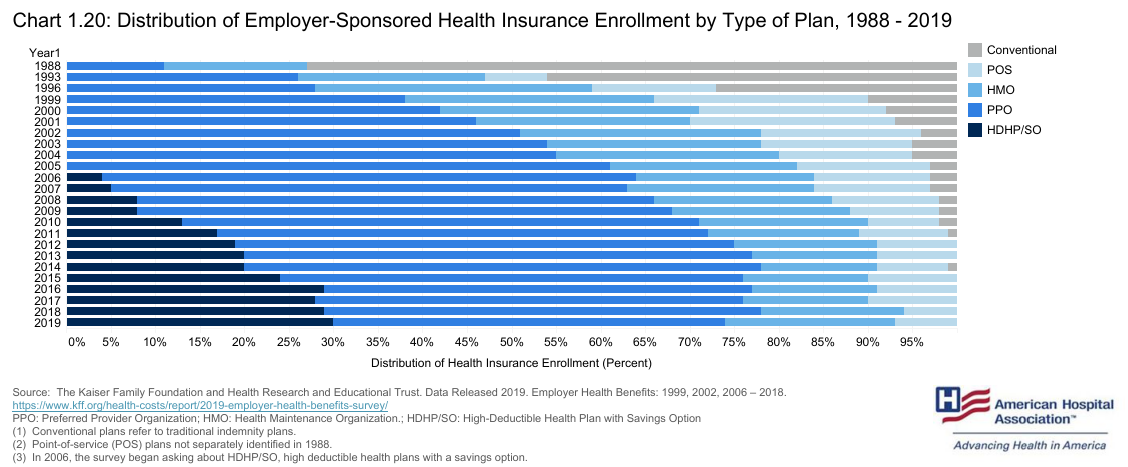
As high deductible plans proliferate, and more information is made available to healthcare consumers, patients will increasingly behave more like the consumers they are in every other aspect of their lives. In this key battle, do you have a winning strategy?
Developing a Price Strategy vs. Managing the Chargemaster
How can a chargemaster be strategic? Said differently, how can charges and price become more “connected” to increase customer acquisition?
First, to be clear, no strategy can impact “fixed” rates, such as Medicare and Medicaid fee schedules. However, a health system’s inability to impact most of its revenue makes it imperative to be strategic about the balance of its revenue.
With that caveat, the advent of CMS’ Hospital Price Transparency rule should be a catalyst to understand the opportunity in your market. Here are a few questions you should ask to understand the opportunities in your market:
- Are your competitors complying with the Price Transparency rule?
If not, it is a sign of their weakness. Either they lack the ability to comply, i.e., they do not have the resources or knowledge to comply, or they are unwilling to comply, i.e., they are hiding something, probably the delta between how much they charge for and the quality of a particular service. Either alternative is an opportunity to engage with consumers about the pricing of your health system. - Do your system’s negotiated rates reflect current and future demand?
There are many hospitals with market-leading rates, but market-lagging share, for specific service lines. Only dominant academic medical centers can charge market-leading rates for routine services by “tagging” their tertiary and quaternary service lines, such as trauma and burn units. It is all too easy for payers and employers to steer patients away from outlier rates for routine ambulatory care, like X-rays. Where are your system’s negotiated rates inconsistent with your market share? Where are your system’s negotiated rates misaligned with future demand for healthcare services?
Even more importantly, you should begin to think about markets and consumers – not patients – like Amazon and Walmart do, with questions like this:
- What is the total available demand for healthcare services from all of the consumers in a defined geographic market?
- What is the future demand for all services from all of the consumers in your market and how will it evolve?
- What healthcare services do the consumers in your market want? How do these services differ across different consumer segments?
- What healthcare services do/will they need? Which of these are you best equipped to handle?
- What are they willing to pay for those services?
- Which services that your system provides are “substitute goods” in a macroeconomic sense? [4]
- How competitive is your system’s price for the substitute healthcare goods in your market?
PART III: Why Health Systems Don’t Know Their Actual Market Share
PART II: Lessons from Nick Saban on Thinking Like a Champion
PART I: Winning a Losing Game, Healthcare Edition
[1] https://www.heinz.cmu.edu/~acquisti/papers/privacy.pdf
[2] https://harpers.org/archive/2020/09/the-big-tech-extortion-racket/
[4] https://www.economicshelp.org/blog/glossary/substitute-goods/
- Winning a Losing Game