Farr’s Law: A Retrospective Analysis
Over the holidays, an executive with one of the nation’s largest health systems asked me about our Farr’s Law posts, wondering whether things had turned out as we anticipated. His question was based in part on the media’s incessant coverage of the number of “positive” cases which has increased in step function with increases in testing, as opposed to the percentage of positive cases, which has ranged between 6-12% per day for months even as daily testing has increased by approximately 2.5X over the same period.[1],[2]
My immediate response was that Farr’s Law focused on the rise and fall of epidemics as reflected in deaths, as opposed to cases or hospitalizations. Even so, the question prompted me to utilize the unique insights from hindsight, which I like to say is 20/15.
To start, I reviewed all of our posts to reflect on the consistent themes. The key question for William Farr was, and for us still is, this:
The problem for solution is, Why do the five deaths become 10, 15, 20, 31, 58, 88 weekly, and then progressively fall through the same measured steps? This difficulty has presented itself in the history of plague and of contagious diseases of every description; but it has generally been disposed of summarily, by the hypothesis that the disease is always introduced from without, and spreads naturally, like a conflagration. When the plague broke out, that is, became epidemic, in Cairo, the Egyptians asserted that it came from Ethiopia; when it decimated Constantinople, it was ascribed to merchandise or vessels from Egypt.
Epidemics appear to be generated at intervals in unhealthy places, spread, go through a regular course, and decline; but of the cause of their evolutions no more is known than of the periodical paroxysms of ague. The body, in its diseases as well as its functions, observes a principle of periodicity; its elements pass through prescribed cycles of changes, and the diseases of nations are subject to similar variations.” [3]
Farr’s observation that “the death rate is a fact; anything beyond this is an inference” is the key to what is now known as Farr’s Law: that epidemics rise and fall at a mathematically predictable rate that can be calculated by a single mathematical formula approximated by a bell-shaped curve.[4],[5]
Our posts repeatedly included this observation:
Of note is that Farr’s Law is generally discussed as if external factors hold constant. As noted by Huang, et al, “[w]hile it may be possible that without human intervention, a solitary outbreak may follow a Gaussian curve, in the modern era of contact suppression, the epidemic curve is shaped by such interventions.”[6] The impact of governmental and societal efforts to “flatten the curve” manifests by shifting cases to the future. The “flattening” is akin to pushing down on the top of the curve with your finger, with a delay in cases manifesting in a “fatter tail” on the right side of the curve.
So, what did we do to apply Farr’s Law to the spread of SARS-CoV-2 in the United States?
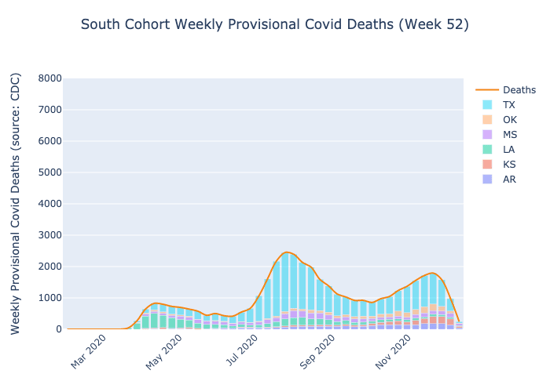
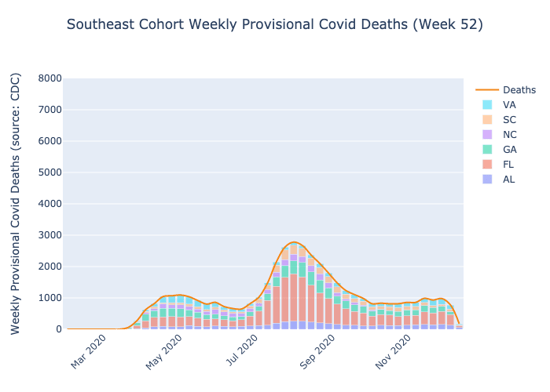
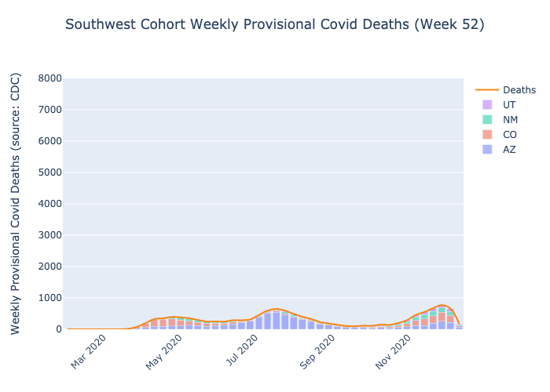
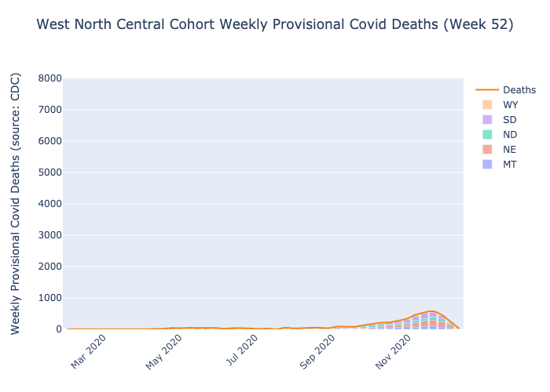
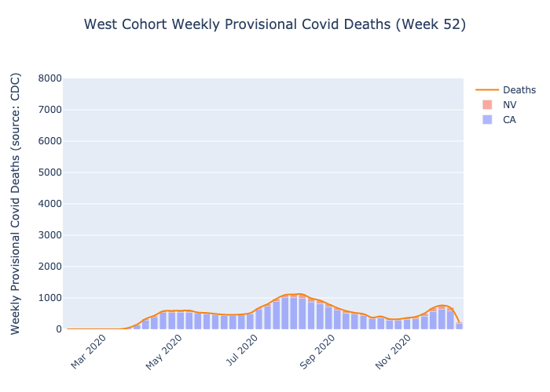
At the end of July, we grouped states (and territories) into months using the day of each state's maximum increase in positive tests from data aggregated by The Covid Tracking Project (https://covidtracking.com). Since no state had a max day in June, we grouped states into three cohorts – April, May and July. We then fit a symmetrical curve to the plot, centering the peak on the cumulative max positive test day for the group.
| Month of Max Increase in Positive Tests | Number of States and Territories |
List of States and Territories |
| April | 12 | Colorado, Connecticut, Delaware, Massachusetts, Michigan, New Jersey, New York, Pennsylvania, Rhode Island, Vermont, Guam, Northern Mariana Islands |
| May | 10 | District of Columbia, Illinois, Iowa, Maine, Maryland, Minnesota, Nebraska, New Hampshire, South Dakota, Virginia |
| June | 0 | None |
| July | 33 | Alabama, Alaska, Arizona, Arkansas, California, Florida, Georgia, Hawaii, Idaho, Indiana, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nevada, New Mexico, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, South Carolina, Tennessee, Texas, Utah, Washington, West Virginia, Wisconsin, Wyoming, Puerto Rico, U.S. Virgin Islands |
How did we do?
To be candid, hindsight suggests that we may have been completely wrong to apply Farr’s Law to the SARS-CoV-2 epidemic. In consideration of the December 29 announcement by World Health Organization (WHO) officials that SARS-CoV-2 “is not necessarily the big one,” the fact that SARS-CoV-2 is closely related to SARS-CoV-1 and MERS, the implications of NIH-sponsored “gain of function” research for “highly pathogenic coronavirus infections,” and the disappearance of influenza from the planet since April, it is perhaps reasonable to suggest that Farr’s Law of Epidemics does not apply at all to SARS-CoV-2.[7],[8],[9],[10] The work of Donald Henderson, M.D., who led the WHO’s effort to eradicate smallpox globally, might endorse this view given the similarity between influenza virus and coronavirus:
Historically, it has been all but impossible to prevent influenza from being imported into a country or political jurisdiction, and there has been little evidence that any particular disease mitigation measure has significantly slowed the spread of flu. The clinical and epidemiologic characteristics of influenza explain why:
-
- The influenza virus is known to spread rapidly from one person to the next, with a second generation of patients occurring within 2–4 days following exposure.
- People infected with influenza may shed virus for 1–2 days before becoming symptomatic.
- Some flu-infected individuals may be asymptomatic and so would not be recognized as being infected. In seasonal flu outbreaks, this group may represent a significant proportion of infected people. Asymptomatic individuals infected with flu have been shown to shed virus, although the extent to which these individuals transmit infection to others is not known.
- Many patients who are symptomatic are not readily diagnosed because their symptoms differ little from individuals with other respiratory illnesses or allergies.” [11],[12],[13]
Putting aside the similarities between SARS-CoV-2 and influenza and the disappearance of influenza from the US since April[14], what does hindsight reveal about our attempt to apply Farr’s Law to SARS-CoV-2? And, based on the most recent data from the National Center for Health Statistics, how accurate was Farr’s Law as a model?
The key thesis in our blog posts was this:
“The application of Farr’s Law to the experience in the United States over the past four months suggests that the widely held belief that the United States is in a “surge” or “resurgence” of Covid-19 is incorrect. As shown in the graphs above, there have been three distinct “outbreaks” of Covid-19 in the United States: one primarily centered in the Northeastern U.S., Colorado and Michigan; another that unfolded in the Upper Midwest and part of the Eastern Seaboard; and the current “outbreak” that is broadly dispersed throughout the rest of the United States, particularly the Sunbelt…with the low, but persistent, case positivity offering support for the notion that the pandemic is now endemic.”[15]
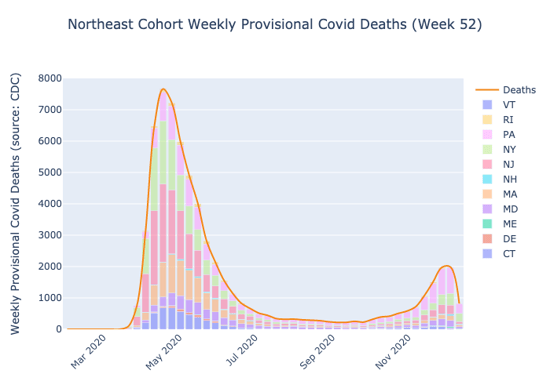
We were correct that there was not one surge, but we were wrong about how many surges there were. Even so, it is striking how much more closely the April cohort seems to reflect Farr’s Law as compared to the July cohort:
What would we do differently with the benefit of hindsight?
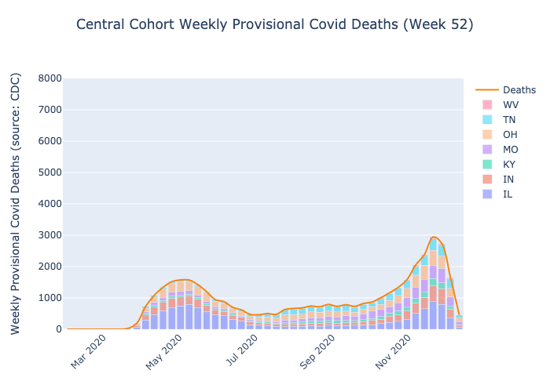
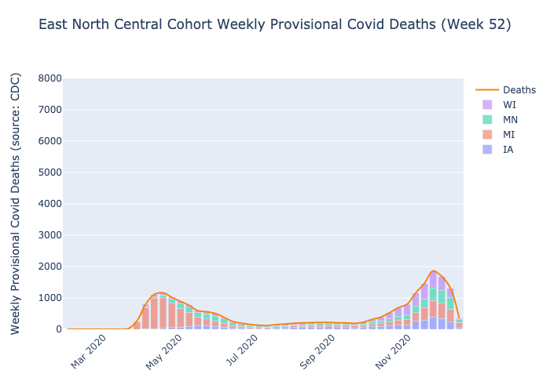
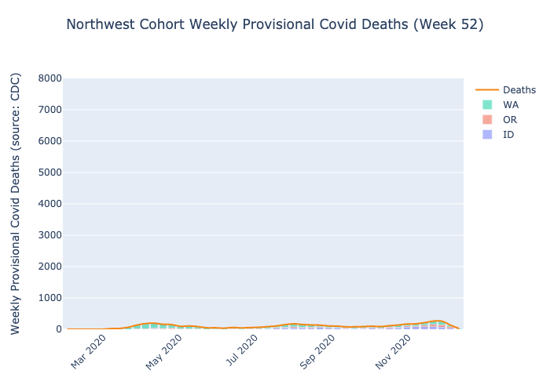
First, we would group our cohorts differently. We were initially skeptical of the correlation of seasonal weather patterns to the “surges” that was identified early in the pandemic, but that correlation is increasingly hard to ignore.[16] Today, we believe that grouping the states according to climate regions identified by the National Centers for Environmental Information provides more validation for Farr’s Law:
Second, in hindsight it is clear that the 50 states with 50 governors and 50 state health departments and countless mayors and county executives and local health departments implemented a variety of policies. While perhaps controversial, a state-level analysis suggests that Farr’s Law was most applicable to two groups of states: those states in which the virus had taken hold before any non-pharmaceutical intervention (NPI) could be implemented, and those states that adhered most closely to traditional views of NPIs as promulgated as recently as 2019 by the WHO and Johns Hopkins.[17],[18] As noted by the Johns Hopkins Center for Health Security in “Preparedness for a High-Impact Respiratory Pathogen Pandemic”:
“A multitude of factors will likely determine how effective NPIs will be, such as the size and geographical range of the outbreak, the specific pathogen, the timing of the outbreak, and the country of occurrence. For example, studies have found that travel restrictions would be less effective once a disease has spread to multiple geographic areas or been introduced to large cities. Additionally, studies show that travel restrictions may have some impact for mild to moderately transmissible pathogens (such as SARS). For highly transmissible pathogens, travel restrictions may only slightly delay the epidemic peak, and the total number of cases would ultimately experience no significant change. While travel restrictions would be unlikely to prevent or substantially slow regional or international transmission of infectious diseases, these measures are commonly used by countries in response to international outbreaks. In recent events such as the 2009 influenza A H1N1 and Ebola in West Africa, many countries implemented travel restrictions, despite evidence that such measures would likely not help. In some instances, these measures have hindered international efforts to contain disease spread.
In the context of a high-impact respiratory pathogen, quarantine may be the least likely NPI to be effective in controlling the spread due to high transmissibility. To implement effective quarantine measures, it would need to be possible to accurately evaluate an individual’s exposure, which would be difficult to do for a respiratory pathogen because of the ease of widespread transmission from infected individuals. Quarantine measures will be least effective for pathogens that are highly transmissible, have short incubation periods, and spread through true airborne mechanisms, as opposed to droplets. As with travel restrictions, quarantine appears to delay the introduction of highly transmissible diseases but not prevent their spread entirely. Quarantine measures also appear more effective with pathogens that had a longer incubation period, such as measles, compared to those with shorter incubation periods, such as influenza. Experiences with quarantine during the West Africa Ebola epidemic highlight the added difficulty of implementing such measures on a large scale, which would only be more difficult in the case of a highly transmissible respiratory disease.”[19]
Perhaps not surprisingly, the WHO and Johns Hopkins recommendations are consistent with the observations of Dr. Henderson, et al. from 2006:
“Over the years, various combinations of these measures have been used under epidemic and pandemic circumstances in attempts to control the spread of influenza. However, there are few studies that shed light on the relative effectiveness of these measures. A historical review of communities in the U.S. during the 1918 influenza pandemic identified only two that escaped serious mortality and morbidity. Both communities had completely cut themselves off for months from the outside world. One was a remote town in the Colorado mountains, and the other was a naval training station on an island in San Francisco Bay. Obviously, this is not a strategy of general utility. Other studies have suggested that, except in the most extreme applications, disease mitigation measures have not had a significant impact on altering the course of an influenza pandemic.”[20]
You can decide for yourself by viewing the state-level analysis here.
Irrespective of the accuracy of our theory about how, or even whether, Farr’s Law applies to SARS-CoV-2, we were correct about the aftermath of the pandemic for hospitals. To wit:
On August 17:
However, one day, hospitals will be the only institution in the world whose "new normal" is the "old normal”, except that the “old normal” will be even more difficult.
On August 31:
In the “new old normal”, certain inconvenient truths will remain. Will regulations and payment policy and patient preference on health care delivery continue to encourage patients to seek care somewhere other than a hospital? Yes. Will the number of commercially insured patients decline? Possibly; in some parts of the country, it already has. Will the prevalence of chronic diseases change? No. Will the Chief Medical Officer need to remind the medical staff that hand-washing hygiene is important? Probably.
On September 15:
To be clear, we believe COVID-19 is a highly contagious virus, and the history of vaccines suggests that it is here to stay. For experienced healthcare executives, this reality is yet another reminder of the Odyssean nature of the job. At the same time, we also believe that history – and data – are important prisms through which to navigate challenging environments.
The recorded history of the world confirms that pandemics do ultimately subside. The question is this: Are you prepared for history to repeat itself? Farr’s Law suggests that COVID-19 could subside rather suddenly, but very predictably. Ask yourself, “Do I have the right market intelligence to position my system, hospital or practice for future growth in the next year or five years?” Any strategic plan developed before March 13, 2020 is probably out of date…
Whether or not you believe Farr’s Law, COVID-19 cannot stop time, and 2021 starts in 107 days. Is your system prepared to return to the “new old normal” of a healthcare market with increased competition for a decreasing number of commercially insured patients whose business you desperately need in order to fulfill your mission?
On October 1:
This sentence from a recent Health Affairs articles should terrify every hospital executive:
"It is too early to determine the extent to which hospitalizations will return to baseline levels. A new, lower norm is conceivable if clinicians become more comfortable with alternatives to inpatient admission, including home-based care with remote monitoring."[21]
Today, we still do not understand completely the periodical paroxysms of ague, but we know a great deal about the facts of COVID-19. We know that the median age of death from COVID-19 is higher than the average life expectancy in the U.S. We know that almost 95% of people over the age of 70 survive COVID-19, and that 99.5% of the people under 70 do. We also know that history has no precedent for predicting pandemics, as William Farr noted almost 200 years ago.
More importantly, we know that healthcare providers face death on a daily basis, and COVID-19 is yet another potentially deadly illness, like cancer and heart disease and diabetes and pneumonia and so many others. But healthcare providers have chosen a profession focused on improving and extending life, not one that is morbidly obsessed with death itself. While I know that the cause of death for my oldest son was Duchenne Muscular Dystrophy, what I mourn is the fact that he is gone, not the cause of his death. And while I think of him every day, I have not allowed his death to keep me from living my life.
The people who have jeopardized the very survival of hospitals throughout America cannot and will not repair the damage they have wrought. We have to do that, and we need to do it now. America’s cities and towns need vibrant hospitals, hospitals that are not barely surviving but thriving. Your community needs your system to thrive. Is your system prepared to thrive? If not, the Dalai Lama reminds us,
“There are only two days in a year that nothing can be done. One is called yesterday, and the other is called tomorrow…”
2021 is finally here, and these observations are truer now than they were when we wrote them. According to the Commonwealth Fund, almost 15M Americans lost commercial health insurance as a result of the pandemic.[22]
Game theory is infrequently, if ever, discussed in healthcare systems, but nothing will have a more profound effect on the performance of America’s hospitals in the next 20 years, because the hospital business is a “negative-sum game.”
“The most difficult problems are negative-sum situations, where the pie is shrinking. In the end, the gains and losses will all add up to less than zero. This means that the only way for a party to maintain its position is to take something from another party, and even if everyone takes his or her share of the "losses," everyone still loses in comparison to what they currently have or really need. This type of situation often sparks serious competition.”[23]
There is no way to win a losing game without competing, but there are a number of ways to compete seriously: winning key battles, cutting losses early, losing less frequently, and losing by a smaller margin than the competition. Winning more or losing less than the competition is virtually impossible without accurate and actionable information.
The “new old normal” is that the pie shrunk by 10% over the last 10 months. Do you have the right information to start winning now?
[1] https://ourworldindata.org/grapher/positive-rate-daily-smoothed?tab=chart&yScale=log&time=2020-06-27..latest&country=~USA
[2] https://covidtracking.com/data/charts/us-daily-tests
[3] Annual report of the Registrar-General of births, deaths, and marriages in England, 1838-1839, pp. 94-95
[4] https://www.oxfordreference.com/view/10.1093/oi/authority.20110803095811145
[5] https://en.wikipedia.org/wiki/Bell_shaped_function
[6] https://www.medrxiv.org/content/10.1101/2020.03.28.20046177v3.full.pdf
[7] https://thehill.com/changing-america/well-being/longevity/531963-the-covid-19-pandemic-may-not-necessarily-be-the-big
[8] https://pubmed.ncbi.nlm.nih.gov/32007145/
[9] https://sph.unc.edu/sph-news/baric-to-lead-10-million-nih-grant/
[10] https://apps.who.int/flumart/Default?ReportNo=6
[11]https://en.wikipedia.org/wiki/Donald_Henderson#:~:text=Donald%20Ainslie%20Henderson%20(September%207,launched%20international%20childhood%20vaccination%20programs
[12] http://www.upmc-biosecurity.org/website/resources/publications/2006/2006-09-15-diseasemitigationcontrolpandemicflu.html
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7607235/
[14] https://www.cdc.gov/flu/weekly/weeklyarchives2020-2021/ILI52.html
[15] https://www.sciencedirect.com/science/article/pii/S2666535220300306
[16] https://www.cebm.net/covid-19/effect-of-latitude-on-covid-19/
[17] https://www.who.int/influenza/publications/public_health_measures/publication/en/
[18] https://apps.who.int/gpmb/assets/thematic_papers/tr-6.pdf
[19] Ibid, p. 57
[20] http://www.upmc-biosecurity.org/website/resources/publications/2006/2006-09-15-diseasemitigationcontrolpandemicflu.html
[21] https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.00980
[22] https://www.commonwealthfund.org/publications/issue-briefs/2020/oct/how-many-lost-jobs-employer-coverage-pandemic





.png?width=550&name=April%20(2).png)
.png?width=550&name=July%20(2).png)